Fatty Liver Without the Booze: Understanding NAFLD, the Modern Metabolic Liver Disease
Introduction
Once considered a rare disorder, Non-Alcoholic Fatty Liver Disease (NAFLD) has quietly emerged as one of the leading causes of chronic liver disease worldwide. NAFLD can develop even in individuals who drink very little alcohol, in contrast to alcohol-related liver disease (ALD).
NAFLD is a metabolic liver disease characterised by excessive fat deposition—mainly triglycerides—in liver cells. The spectrum of this disease ranges from simple steatosis to non-alcoholic steatohepatitis (NASH), which can cause inflammation and scarring, sometimes progressing to cirrhosis and liver cancer

NAFLD vs ALD: Two Faces of the Same Coin
Two major conditions stand out:
Non-Alcoholic Fatty Liver Disease (NAFLD)
Alcohol-Related Fatty Liver Disease (ALD)
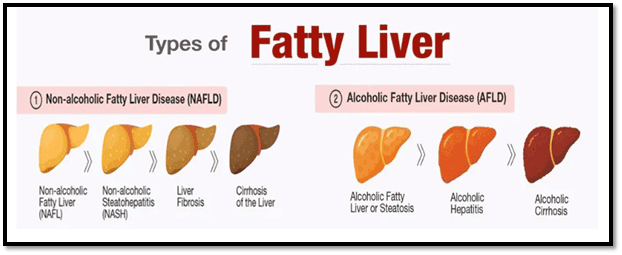
Although their origins differ from NAFLD from metabolic issues and lifestyle factors, ALD from alcohol intake both involve fat buildup, inflammation, and gut imbalance.
The gut microbiome plays a major role in digestion, immunity, and overall metabolic health. While both look similar under a microscope, their fatty liver causes differ.
• In ALD, alcohol breaks down into toxic compounds that inflame liver cells.
• In NAFLD, excess calories, refined carbs, and foods that cause fatty liver overwhelm the liver, especially when metabolism and insulin balance are disturbed.
Both can progress to cirrhosis or liver cancer, but NAFLD often develops silently, with NAFLD symptoms appearing late or being found during routine tests.
LIFESTYLE & DIET: The Heart of the Problem
NAFLD is often seen as the liver’s reaction to an unhealthy lifestyle, where poor diet and low activity disturb metabolism and promote fatty liver disease. Every bite and sip directly affects liver fat.
What Drives Fatty Liver?
1. Refined Carbohydrates and Sugar
Excess calories from sugary foods, soft drinks, and packaged juices trigger de novo lipogenesis in your body’s internal fat-making process. These foods that cause fatty liver lead to rapid fat buildup, especially when insulin balance is affected.
2. Sedentary Lifestyle
A sedentary lifestyle slows fat oxidation and reduces insulin sensitivity, causing excess glucose to convert into fat. Low physical activity weakens metabolism, making it easier for fatty liver disease to progress.
3. Obesity and Visceral Fat
Excess abdominal fat releases free fatty acids directly into the liver, increasing fat deposition. This visceral fat is a major contributor to fatty liver causes, especially when digestion and gut flora are imbalanced.
Research shows that the quality of food matters more than calories. Even people with normal weight can develop NAFLD if they follow a Western-style diet high in sugar and processed fats, common foods that cause fatty liver.
Management of NAFLD: Turning the Tide
If you are diagnosed with NAFLD, managing it early is essential. With the right lifestyle changes and diet, early-stage NAFLD can be reversed.
1. Weight Loss
Weight loss is one of the most effective ways to reduce fatty liver disease.
A 7–10% drop in body weight can improve liver fat, inflammation, and fibrosis.
Even a 3–5% reduction helps lower fat buildup by improving metabolism, insulin response, and overall immunity.
2. Exercise as Medicine
Regular exercise improves insulin sensitivity and boosts fat metabolism, helping the body burn excess fat more efficiently.
Studies show that:
• 150 minutes of moderate exercise, or
• 75 minutes of vigorous activity per week
can significantly reduce liver fat even without major weight loss.
A mix of aerobic workouts and resistance training gives the best results, improving muscle energy use and supporting overall lifestyle health.
3. The Protective Plate
Along with staying active, the right foods support weight control, better metabolism, and lower fatty liver disease risk.

Vegetables
Choose non-starchy veggies like cabbage, carrots, cauliflower, okra, radish, spinach, tomato, zucchini, eggplant, and salad greens. These support healthy digestion and gut flora.
Grains
Pick complex carbs such as brown rice, oats, quinoa, and millets to stabilise insulin levels.
Proteins
Include plant-based sources like lentils, beans, tofu, and edamame—or lean proteins like fish and skinless chicken.
Healthy Fats
Use extra-virgin olive oil, avocados, nuts, and seeds in moderation to support immunity and metabolic balance.
Foods and Beverages to avoid
Sugary foods and sweetened beverages
Alcohol (can worsen fatty liver causes)
Too many starchy vegetables paired with refined grains
Red and processed meat
Whole-fat dairy
Foods high in saturated and trans fats
4. Medical Monitoring
Regular medical monitoring is essential to track liver health, metabolism, and risks linked to fatty liver disease. It also helps detect issues early, especially when NAFLD symptoms are silent.

Recommended Tests:
Liver enzyme levels (ALT, AST)
Ultrasound or Fibro-Scan to track steatosis and fibrosis
Evaluation of associated conditions: diabetes, hypertension, dyslipidaemia
5. Additional Support
Long-term lifestyle changes can be difficult, especially when managing fatty liver disease. Support from dietitians, healthcare professionals, group programs, and counselling can help you stay consistent and improve overall metabolism, digestion, and immunity.
Prevention: Start Before the Liver Protests
Preventing NAFLD begins with maintaining a healthy lifestyle and protecting your metabolism before issues appear.
Keep a healthy waist size (under 90 cm for men, 80 cm for women).
Limit sugary drinks and ultra-processed foods—common foods that cause fatty liver.
Exercise regularly and prioritise good sleep.
Manage stress and screen early for diabetes to support insulin balance.
Encourage balanced diets and active routines at a community level
Gut microbiome testing can also offer insights into liver and overall health.
Raising awareness can reduce the growing burden of fatty liver disease globally.
Gut–Liver Axis: The Hidden Connection
The gut and liver are deeply linked through digestion, metabolism, and immunity. Nutrients, toxins, and microbial by-products move from the intestines to the liver through the portal vein, meaning your gut flora directly influences fatty liver disease risk and overall liver health.
The Role of Gut Microbiota
Disturbances in the gut microbiome can worsen NAFLD in several ways:
• Increased intestinal permeability allows toxins to enter the liver, causing inflammation.
• Altered bile acid metabolism affects fat digestion and insulin signalling.
• Changes in short-chain fatty acid production impact fat storage, digestion, and overall immunity, increasing the risk of fatty liver disease.
Healing Through Gut
Modulating the gut microbiota is a promising way to manage fatty liver disease.
High-fibre foods and prebiotics like oats, bananas, garlic, and legumes help nourish good gut flora and support healthy digestion.
Probiotics and fermented foods such as curd, kefir, and kimchi may reduce liver enzyme levels and lower fat buildup by improving immunity and metabolism.
While future treatments may include microbiome-targeted therapies or faecal microbiota transplantation, a gut-friendly diet remains one of the safest and most effective strategies today.
Conclusion: Your Liver Reflects Your Lifestyle
NAFLD is largely a lifestyle-driven condition shaped by poor diet, inactivity, stress, weak metabolism, and disrupted digestion. While both NAFLD and ALD affect the same organ, NAFLD is a sign that your metabolic health and daily habits need attention.
The good news? Early-stage fatty liver disease is reversible.
A nutrient-rich diet, regular exercise, better insulin control, and a healthy gut flora can restore liver health and boost overall immunity.
Remember, liver health is not just about what you drink
“It’s how you live and eat.”
-Nishmitha Bhandary
Reference
Arab, J. P., Arrese, M., & Trauner, M. (2018). Recent insights into the pathogenesis of nonalcoholic fatty liver disease. Annual Review of Pathology: Mechanisms of Disease, 13(1), 321–350. https://doi.org/10.1146/annurev-pathol-020117-043617
Chalasani, N., Younossi, Z., Lavine, J. E., Charlton, M., Cusi, K., Rinella, M., Harrison, S. A., Brunt, E. M., & Sanyal, A. J. (2012). The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance by the American Association for the Study of Liver Diseases. Hepatology, 55(6), 2005–2023. https://doi.org/10.1002/hep.25762
Zhou, J., Zhou, F., Wang, W., Zhang, X. J., Ji, Y. X., Zhang, P., She, Z. G., Zhu, L., Cai, J., & Li, H. (2023). Epidemiological trends of NAFLD and NASH: A global perspective. Frontiers in Medicine, 9, 10029946. https://pmc.ncbi.nlm.nih.gov/articles/PMC10029946/.
Safari, Z., & Gérard, P. (2019). The links between the gut microbiome and non-alcoholic fatty liver disease (NAFLD). Fundamental & Clinical Pharmacology, 33(4), 462–477. https://link.springer.com/article/10.1007/s00018-019-03011-w
Tilg, H., & Moschen, A. R. (2010). Evolution of inflammation in nonalcoholic fatty liver disease: The multiple parallel hits hypothesis. Hepatology, 52(5), 1836–1846. https://doi.org/10.1002/hep.24001
Buzzetti, E., Pinzani, M., & Tsochatzis, E. A. (2016). The multiple-hit pathogenesis of non-alcoholic fatty liver disease (NAFLD). Metabolism, 65(8), 1038–1048. https://pmc.ncbi.nlm.nih.gov/articles/PMC6334080/
Leung, C., Rivera, L., Furness, J. B., & Angus, P. W. (2016). The role of the gut microbiota in NAFLD. Nature Reviews Gastroenterology & Hepatology, 13(7), 412–425. https://pmc.ncbi.nlm.nih.gov/articles/PMC7468507/
Carstensen, J., & Balakrishnan, M. (n.d.). Non alcoholic fatty liver disease.