The MicroByte Series -Staphylococcus epidermidis: A Double-Edged Sword
History
Staphylococcus epidermidis, whose name comes from ‘staphyl’ meaning, grape bunch-like appearance under a microscope, ‘coccus’ which indicates the round shape of the cells, and ‘epidermidis’ from its strong association with the skin. However, this bacteria went by several names prior. In 1884, Friedrich Rosenbach differentiated it from S. aureus, naming it Staphylococcus albus, due to its white appearance. Later, when bacteria were split according to their colony colours, Winslow and Winslow proposed its renaming to Albococcus epidermidis, acknowledging its role in the skin. It was later grouped back with the Staphylococcus genus, and it remains Staphylococcus epidermidis to this date.
Habitat
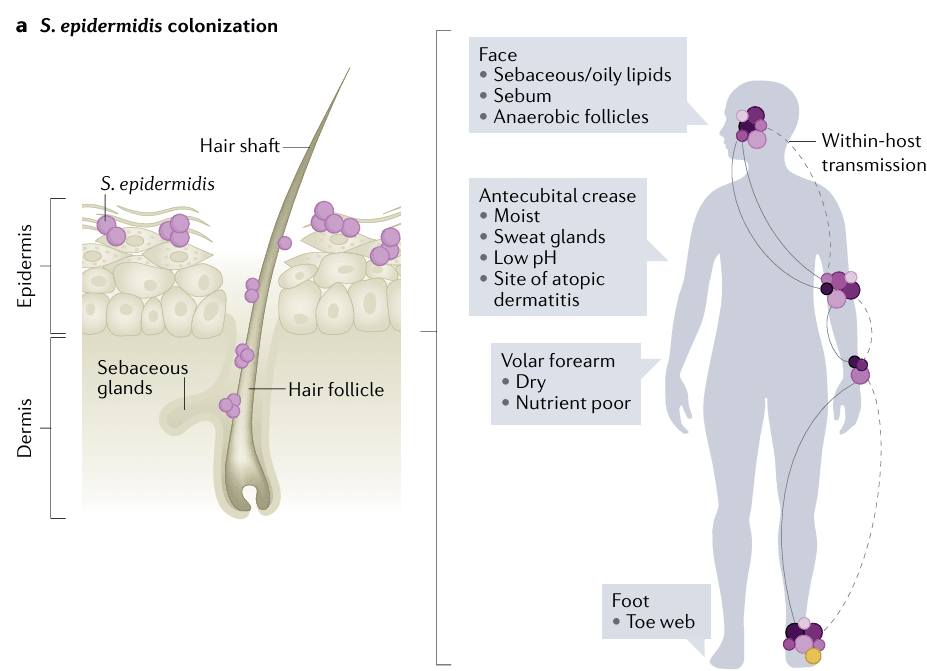
S. epidermidis, as its name suggests, can live in all types of skin sites, be it dry, sebaceous, or oily, but prefers moist sites. In terms of body sites, it is found in the armpit, nostrils, and face, as it is adapted to also thrive in mucous membranes.
Health Benefits
S. epidermidis has several useful properties that allow it to inhabit the skin and be part of the skin microbiome. It has anchoring proteins, which allows it to attach to the skin’s surface, where it plays important roles throughout a person’s lifetime- it is believed we first encounter this microbe in the womb. During childhood, it ‘trains’ the immune system. This ‘training’ allows the immune system to recognise the normal microbiota, and only react against harmful microbes which can cause infection and disease. It can also produce enzymes to increase ceramide levels in the skin, which help maintain its hydration. Interestingly, it also competes with Staphylococcus aureus, known to be associated with severe infections and skin conditions, by secreting antimicrobial compounds, or by recruiting the immune cells. S. epidermidis also plays a similar immune-modulating role in the nasal microbiome, and may be involved in fighting off respiratory infections.
Applications
The positive roles played by S. epidermidis in skin health are beginning to be harnessed through the development of probiotics. An exploratory study showed that isolated S. epidermidis from a human’s own facial skin, when re-applied, improved skin barrier integrity and hydration. It has also been proposed that introduction of this commensal to the nostril during respiratory infection could help in faster recovery due to its ability to compete with pathogens and harness the immune system. Certain strains of S. epidermidis have also been shown to reduce S. aureus, when applied on patients with atopic dermatitis- a condition typically known to be made worse by this pathogen. Further research is needed to identify strains of S. epidermidis that can exert positive effects while posing minimal risk.
Risks
Despite its several interesting and beneficial properties, and being low-virulent, S. epidermidis is also known to cause infection, being one of the leading causes of hospital-acquired infections. It commonly enters the body through the process of implanting prosthetics and medical devices, or IV lines and injections, due to its presence on the skin. These infections must be identified and treated in a timely manner through appropriate culture analysis and antibiotic treatment.
Microbe Profile
Shape : Cocci
Gram nature : Gram Positive
Spore formation : No
Biofilm formation : Yes
Oxygen requirement : Facultative anaerobe
Optimal temperature : 30–37°C
Optimal pH : 5-7
Nutrient usage : Glucose, Lactate
Taxonomic classification
Domain : Bacteria
Phylum : Bacillota
Class : Bacilli
Order : Bacillales
Family : Staphylococcaceae
Genus : Staphylococcus
Species : Staphylococcus epidermidis
-Antara Arvind
References
Licitra G. (2013). Etymologia: Staphylococcus. Emerging Infectious Diseases, 19(9), 1553. https://doi.org/10.3201/eid1909.ET1909
Otto M. (2009). Staphylococcus epidermidis--the 'accidental' pathogen. Nature reviews. Microbiology, 7(8), 555–567. https://doi.org/10.1038/nrmicro2182
Severn, M. M., & Horswill, A. R. (2023). Staphylococcus epidermidis and its dual lifestyle in skin health and infection. Nature reviews. Microbiology, 21(2), 97–111. https://doi.org/10.1038/s41579-022-00780-3
Kim, H.J., Jo, A., Jeon, Y.J. et al (2019). Nasal commensal Staphylococcus epidermidis enhances interferon-λ-dependent immunity against influenza virus. Microbiome 7, 80. https://doi.org/10.1186/s40168-019-0691-9
Nodake, Y., Matsumoto, S., Miura, R., Honda, H., Ishibashi, G., Matsumoto, S., Dekio, I., & Sakakibara, R. (2015). Pilot study on novel skin care method by augmentation with Staphylococcus epidermidis, an autologous skin microbe--A blinded randomized clinical trial. Journal of dermatological science, 79(2), 119–126. https://doi.org/10.1016/j.jdermsci.2015.05.001
Ortega-Peña, S., Rodríguez-Martínez, S., Cancino-Diaz, M. E., & Cancino-Diaz, J. C. (2022). Staphylococcus epidermidis Controls Opportunistic Pathogens in the Nose, Could It Help to Regulate SARS-CoV-2 (COVID-19) Infection? Life, 12(3), 341. https://doi.org/10.3390/life12030341
Teruaki Nakatsuji et al. (2017), Antimicrobials from human skin commensal bacteria protect against Staphylococcus aureus and are deficient in atopic dermatitis.Sci. Transl. Med.9, eaah4680.DOI:10.1126/scitranslmed.aah4680
Lee E, Anjum F. Staphylococcus epidermidis Infection. [Updated 2023 Apr 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK563240/
Chiara Montanari, Diana I. Serrazanetti, et al (2015), New insights in thermal resistance of staphylococcal strains belonging to the species Staphylococcus epidermidis, Staphylococcus lugdunensis and Staphylococcus aureus, Food Control, Volume 50, Pages 605-612, ISSN 0956-7135, https://doi.org/10.1016/j.foodcont.2014.09.039.
Pedroza-Dávila, U., Uribe-Alvarez, C., Morales-García, L., Espinoza-Simón, E., Méndez-Romero, O., Muhlia-Almazán, A., Chiquete-Félix, N., & Uribe-Carvajal, S. (2020). Metabolism, ATP production and biofilm generation by Staphylococcus epidermidis in either respiratory or fermentative conditions. AMB Express, 10(1), 31. https://doi.org/10.1186/s13568-020-00966-z.
Skovdal, S. M., Jørgensen, N. P., & Meyer, R. L. (2022). JMM Profile: Staphylococcus epidermidis. Journal of Medical Microbiology, 71(10). https://doi.org/10.1099/jmm.0.001597.