5 Common Signs Linked to Poor Gut Health
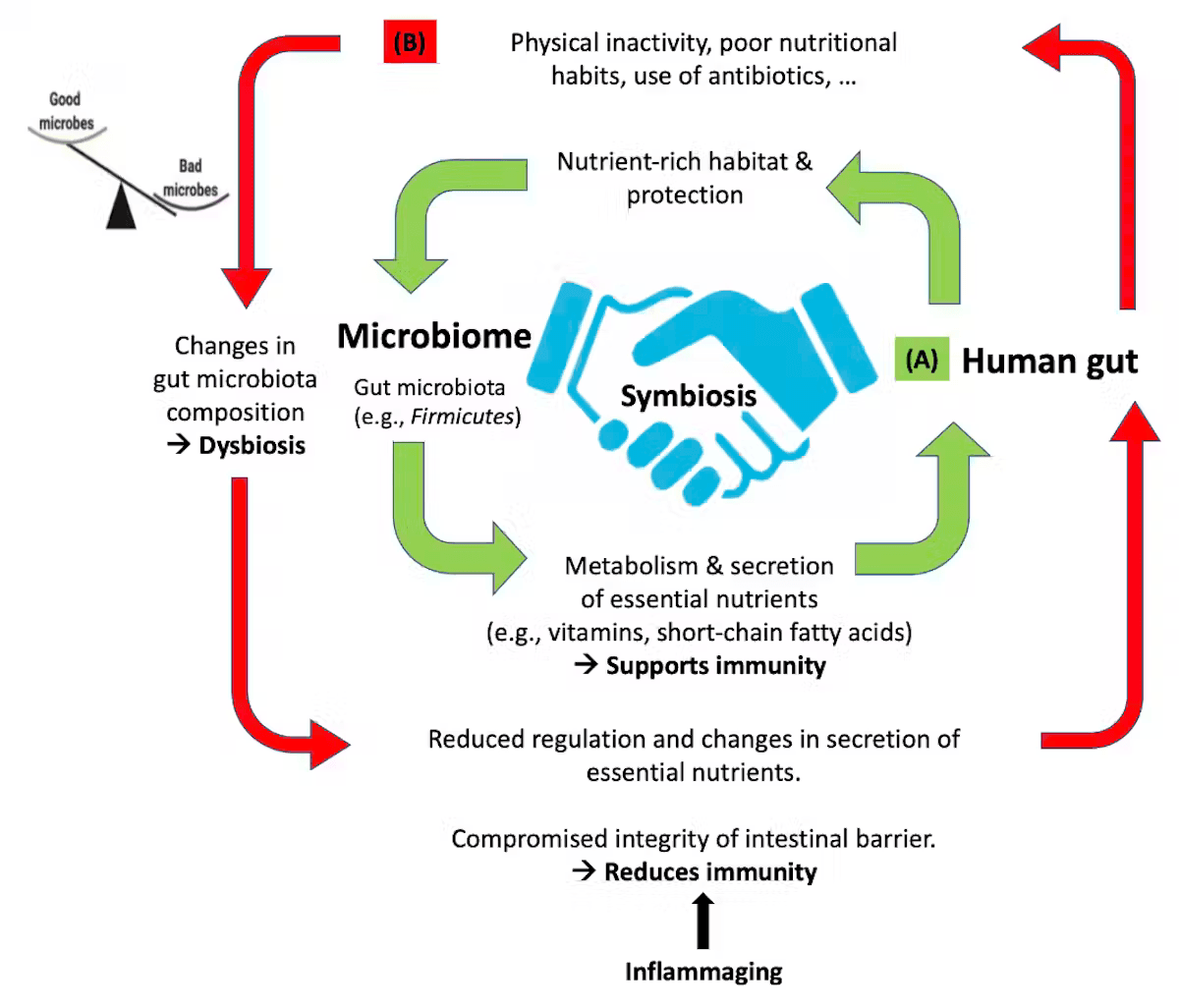
Our gut does a lot more work than just digesting food. It plays an important role in our health from supporting the immune system to influencing our mood and energy levels. Poor gut health can quietly and gradually affect our daily life in ways that we might not immediately notice. The key to maintaining a healthy gut balance lies in the interaction between the host and gut microbes. This interaction plays a crucial role in maintaining a well balanced, diverse gut microbiome.
Diet, lifestyle, age and environment influence the gut microbial composition . Most of the time, gut microbes coexist peacefully with us. However, if there is any disruption of this balance, these microbes can start causing problems. Even if we eat the healthiest foods, the nutrient absorption can be compromised because of such imbalances.
Balanced interaction between the human gut and microbiome-In a healthy state, the gut gives nutrients and shelter to microbes, which in turn support the immune system. However poor diet, inactivity or over use of antibiotics can disrupt this balance.
5 Signs of Poor Gut Health
1. Stomach Upset
Frequent bloating, heartburn, diarrhoea, gas, constipation and acidity is associated with poor gut health. While occasional symptoms are normal, recurring discomforts might be a sign of dysbiosis. Gut bacteria are involved in breaking down food, but when disrupted, they can cause excess fermentation and gas production especially after consuming fibre or sugar alcohols (e.g. sorbitol).
Inflammation or changes in the nerve and muscle function in the intestines along with the gas production by bacteria can make the bloating worse. Studies show that patients with Irritable Bowel Syndrome (IBS) have more gas producing bacteria and fewer beneficial bacteria like the members of the genus Bifidobacterium, phyla Clostridia and Bacteroidetes ,while bacteria belonging to the family Ruminococcaceae were found to be overrepresented.
2. Food Intolerance and Sensitivities
A healthy gut microbiome is responsible for strengthening and maintaining the gut barrier integrity. When this integrity is compromised it leads to the condition called ‘leaky gut’, where the undigested food particles, toxins and microbes enter the bloodstream, overstimulating the immune system, causing inflammation which can lead to food sensitivities or allergies. Factors like poor diet, stress, antibiotics can cause gut microbiome imbalance which can impair the barrier integrity and break down immune tolerance. Higher levels of Proteobacteria and Fusobacteria associated with dysbiosis, can further weaken the barrier integrity.
In children, high Enterobacteriaceae/Bacteroidaceae ratio were linked to food sensitization, which could be associated with the development of food allergies. Beneficial bacteria like Clostridiales and Lactobacillales produce short chain fatty acids(SCFA’s) like butyrate and propionate and confers anti-inflammatory effects and strengthens the gut barrier integrity. In addition, they also aid in preventing food allergies and promoting immune tolerance.
3. Obesity and Poor Sleep
Recent research shows that obesity might be linked to an imbalance in gut microbiome. This can affect how our body processes nutrients, stores fat, responds to inflammation and produces energy. For instance , the ratio of Firmicutes to Bacteroidetes is often higher in obese people. This is associated with increased energy absorption from food and more fat storage. Diets high in fat can lead to an increase in Proteobacteria, a group that includes some harmful bacteria and reduces beneficial bacteria like Faecalibacterium, Ruminococcus and Oscillospira. Certain gut bacteria can influence the expression of the proteins like ANGPTL4 that are responsible for regulating fat storage. Beneficial strains like Lactobacillus paracasei F19 and Bifidobacterium lactis BB12 are found to promote ANGPTL4 levels and help to reduce fat storage and support a healthier metabolism.
Gut health affects sleep through the gut-brain axis. Reduced number of SCFA producers like Lactobacillus, Bifidobacterium, Faecalibacterium and Roseburia are associated with leaky gut and inflammation that can negatively impact sleep quality. Poor gut health can interfere with the production of serotonin - a neurotransmitter. Over 90% of serotonin is produced in the gut and plays a key role in regulating sleep and mood. Gut bacteria are also found to influence the expression of circadian genes like BMAL1 and CRY1, which regulate the internal clock of our body and any disruptions in these genes, can further worsen sleep quality and metabolism .
4. Skin Diseases
Poor gut health can worsen conditions like acne, eczema and psoriasis. SCFA produced by gut microbes was found to promote and regulate differentiation of regulatory T cells (Tregs), thus reducing inflammation and supporting skin barrier function. Studies have shown that decreased abundance of SCFA producers like Faecalibacterium prausnitzii and Bacteroides fragilis are associated with the inflammatory skin diseases. Psoriasis shares common dysbiosis features with IBS including low microbial diversity and impaired SCFA-mediated immune regulation. Therefore, maintaining gut microbial balance is important for skin immune homeostasis and prevention of inflammatory skin disorders.
5. Sugar Cravings
Gut microbes can also influence our food preferences and cravings especially for sugar. Certain gut bacteria and yeasts thrive on sugar as their primary energy source. For their own survival, these microbes can even manipulate our appetite and eating behaviour and force us to consume more sugar. One way this happens is through the production of neurotransmitters like dopamine and serotonin. These chemicals are involved in mood and reward. When we consume sugar, it stimulates dopamine release and creates a sense of satisfaction . Certain gut microbes may enhance this feedback loop which makes us crave sugar more. Also, when the gut microbiome is imbalanced, it can disrupt the regulation of hormones like ghrelin which stimulates hunger and leptin, which signals fullness. This may lead to uncontrolled hunger and persistent sugar cravings . A well-known example is Candida albicans, a yeast that naturally lives in the gut. In small amounts, it is harmless, but when it overgrows, it thrives on sugar and often causes intense cravings .
Recommending no sugar can make you feel low, but trust us ‘NoSugar’ can also make your tiny residents and you happy with the best offers!
-Ganesh.S
REFERENCES
Crucillà, S., Caldart, F., Michelon, M., Marasco, G., & Costantino, A. (2024). Functional abdominal bloating and gut microbiota: an update. Microorganisms, 12(8), 1669. https://doi.org/10.3390/microorganisms12081669
Fusco, W., Lorenzo, M. B., Cintoni, M., Porcari, S., Rinninella, E., Kaitsas, F., Lener, E., Mele, M. C., Gasbarrini, A., Collado, M. C., Cammarota, G., & Ianiro, G. (2023). Short-Chain Fatty-Acid-Producing bacteria: key components of the human gut microbiota. Nutrients, 15(9), 2211. https://doi.org/10.3390/nu15092211
Poto, R., Fusco, W., Rinninella, E., Cintoni, M., Kaitsas, F., Raoul, P., Caruso, C., Mele, M. C., Varricchi, G., Gasbarrini, A., Cammarota, G., & Ianiro, G. (2023). The role of gut microbiota and leaky gut in the pathogenesis of food allergy. Nutrients, 16(1), 92. https://doi.org/10.3390/nu16010092
Noor, J., Chaudhry, A., Batool, S., Noor, R., & Fatima, G. (2023). Exploring the impact of the gut microbiome on obesity and weight loss: a review article. Cureus. https://doi.org/10.7759/cureus.40948
Lin, Z., Jiang, T., Chen, M., Ji, X., & Wang, Y. (2024). Gut microbiota and sleep: Interaction mechanisms and therapeutic prospects. Open Life Sciences, 19(1). https://doi.org/10.1515/biol-2022-0910
Salem, I., Ramser, A., Isham, N., & Ghannoum, M. A. (2018). The gut microbiome as a major regulator of the Gut-Skin axis. Frontiers in Microbiology, 9. https://doi.org/10.3389/fmicb.2018.01459
Mahmud, M. R., Akter, S., Tamanna, S. K., Mazumder, L., Esti, I. Z., Banerjee, S., Akter, S., Hasan, M. R., Acharjee, M., Hossain, M. S., & Pirttilä, A. M. (2022). Impact of gut microbiome on skin health: gut-skin axis observed through the lenses of therapeutics and skin diseases. Gut Microbes, 14(1). https://doi.org/10.1080/19490976.2022.2096995
Han, H., Yi, B., Zhong, R. et al. From gut microbiota to host appetite: gut microbiota-derived metabolites as key regulators. Microbiome 9, 162 (2021). https://doi.org/10.1186/s40168-021-01093-y
Anita. (2023, April 16). Candida Overgrowth: the Sugar-Yeast Connection. Anita Wang, MD. https://www.anitawangmd.com/candida-overgrowth