- April 10, 2024
- Siddhi Talgaonkar
- Microbiome and Disease
Antibiotics: Clearing the Infection or Clearing Out Your Gut? Navigating the Impact on Gut Health
Antibiotics revolutionized the fight against infectious diseases, altering the landscape of modern medicine. Their discovery, which provided a powerful weapon against bacterial illnesses that once posed serious dangers to human life, represented a turning point in the history of healthcare.
Antibiotics have made diseases such as pneumonia, TB, and many others more treatable, lowering mortality rates and improving public health worldwide. The capacity to rapidly eliminate bacterial pathogens and efficiently cure infections transformed medical procedures, resulting in notable improvements in patient care and results.
The widespread use of antibiotics raises new concerns, including antibiotic resistance as bacteria develop defenses against them. Additionally, antibiotics can harm the gut flora, disrupting its delicate balance. This ecosystem in our digestive tract plays a crucial role in immune function, food absorption, and digestion, affecting overall health. Broad-spectrum antibiotics, while targeting harmful bacteria, can also disturb the gut microbiome, potentially impacting long-term human health.
Impact of Antibiotics on Gut Health
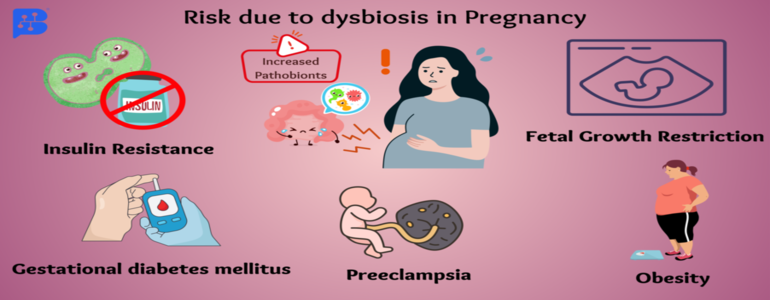
On Mothers and Baby: Antibiotics during pregnancy and breastfeeding can harm both mother and baby by upsetting the balance of beneficial gut bacteria. Research suggests that these medications can alter the baby's gut flora, potentially leading to digestive issues like colitis later in life. Additionally, administering antibiotics during childbirth can compromise the baby's immune system and overall health.
Antibiotics are frequently given to premature babies in the NICU because they are more susceptible to contracting infections. However, administering these strong antibiotics can alter the variety of beneficial bacteria in the baby's gut, making it less diverse and reducing the number of different types of bacteria. Also, this may increase the bacteria's resistance to drugs, which could be dangerous. These alterations in gut flora have been connected to severe health issues in preterm infants, such as necrotizing enterocolitis, a dangerous intestinal disorder, and late-onset sepsis, a form of infection. Other than that, it can increase Enterococcus and decrease beneficial bacteria like Bifidobacteria and Bacteroidetes.
On Adults: The use of antibiotics in adults can cause notable disruptions in the makeup of the gut microbiota, which lowers the diversity and richness of microbial communities. It has been demonstrated that even brief antibiotic courses have long-lasting impacts on the gut microbiota, with the establishment of antibiotic-resistant strains and an incomplete restoration of the microbial makeup. Furthermore, different antibiotics have distinct effects on the gut microbiota; bacteriostatic medications encourage the growth of Gram-negative bacteria, whereas bactericidal medications encourage the growth of Gram-positive bacteria.
Overall, indiscriminate antibiotic use across life stages offers severe health risks to humans by altering the delicate balance of the microbiota and encouraging the emergence of antibiotic resistance.
Clinical Consequences of Antibiotic:
Short-Term Consequences: Excessive antibiotic use can lead to immediate consequences like antibiotic-associated diarrhea (AAD), caused by disrupting the balance of microorganisms in the stomach. This disruption can persist after stopping the medication, potentially leading to Clostridium difficile-associated diarrhea (CDAD), a more serious condition that can be harmful, especially in elderly individuals with weakened immune systems.
Long-Term Consequences: Misusing antibiotics, especially in infancy and childhood, can have significant long-term health consequences. It disrupts the gut microbiota, increasing the risk of obesity, asthma, allergies, and inflammatory bowel disease (IBD) later in life. Studies show that children given antibiotics at a young age are more likely to develop these illnesses compared to those who are not.
Effect of antibiotic-induced gut alternation on Immune and Metabolic Health: Infection Susceptibility- Changes in the gut microbiota enhance infection susceptibility, which is a major concern. An imbalance in the gut's bacterial population can increase the risk of intestinal illnesses. This may occur as a result of opportunistic organisms becoming more aggressive or dangerous pathogens taking control. For instance, diarrhea brought on by antibiotics, which is frequently brought on by Clostridium difficile, can get severe and recurrent. Changes in the gut flora can also make bloodstream infections more common in people with compromised immunity. Premature infants, who are frequently given antibiotics, are more vulnerable to sepsis, a life-threatening illness linked to changes in their gut microbes. These dangers emphasize how crucial it is to maintain a balanced gut microbiota to prevent infections.
Impaired Tolerance and Immune Homeostasis: Antibiotic usage can alter the gut flora, disrupt immunological homeostasis, and have long-term health implications. Early exposure to antibiotics has been associated with a higher incidence of autoimmune, inflammatory, and atopic illnesses. Research indicates correlations between the use of antibiotics and ailments such as allergic reactions, inflammatory bowel illnesses, and asthma. However, new studies show that exposure to antibiotics, especially broad-spectrum antibiotics, might cause problems like asthma in a dose-dependent manner. Furthermore, a mother's use of antibiotics throughout her pregnancy may raise her child's risk of developing atopic illnesses. Microbiota changes are also associated with irritable bowel syndrome (IBS), which frequently occurs after gastrointestinal illnesses and may be impacted by antibiotic use.
Deregulated Metabolism: Many metabolic problems can arise from disruptions in host metabolism brought on by antibiotic-induced changes in the gut microbiota. Obesity has been linked to changes in the gut microbiota, including decreased diversity and changes in bacterial genes and metabolic pathways that promote energy extraction from food. By increasing persistent low-grade inflammation, antibiotics can worsen the development of metabolic syndrome, a group of disorders that includes fatty liver disease, cardiovascular disease, and type 2 diabetes. Moreover, epidemiological research and mice models have demonstrated that antibiotics raise the risk of type 1 diabetes, an autoimmune illness. These results emphasize the intricate connection between gut microbiota, antibiotic usage, and metabolic health and highlight the significance of sparingly using antibiotics to reduce metabolic risks.
How do you keep your gut healthy while taking antibiotics?
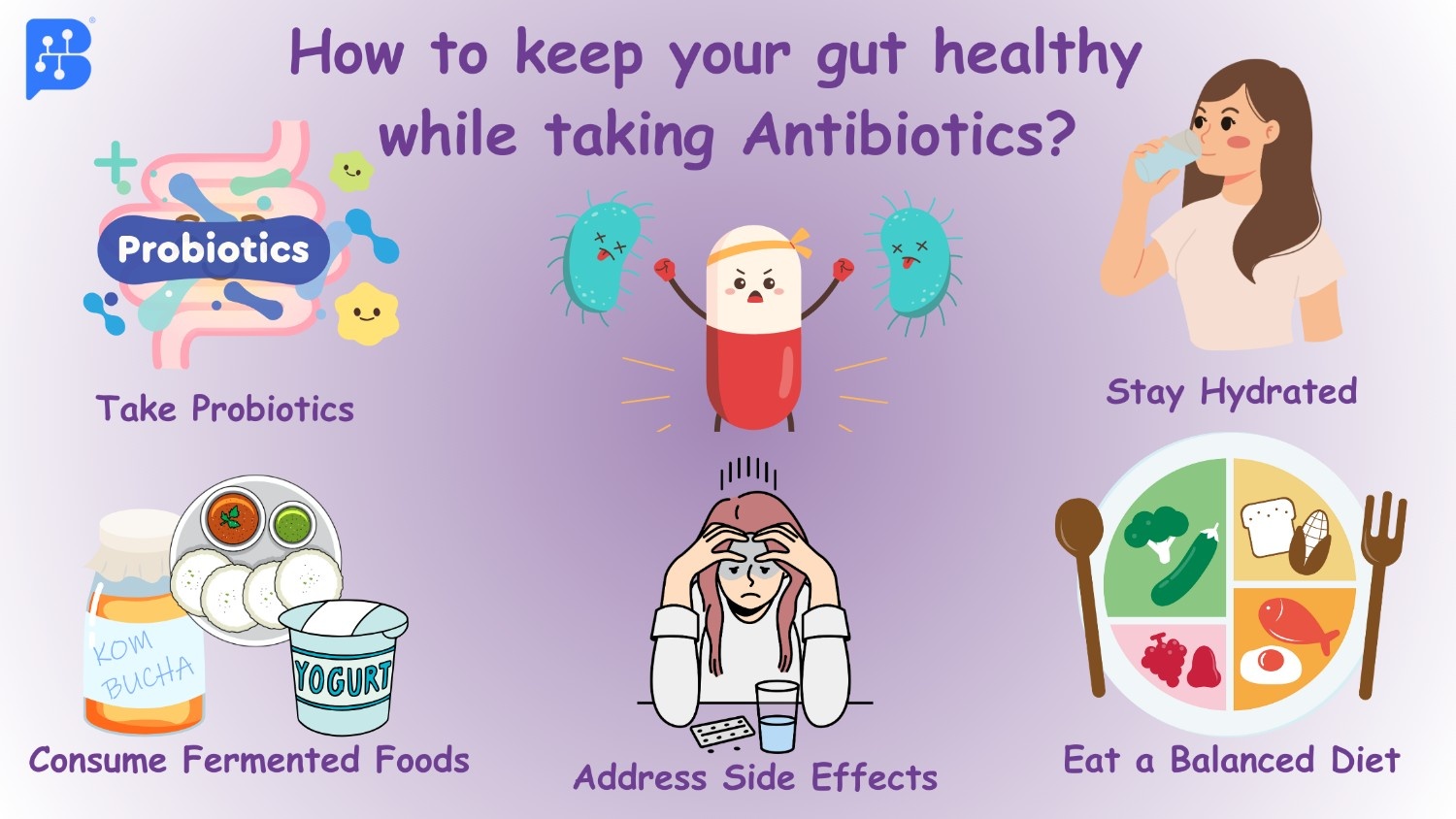
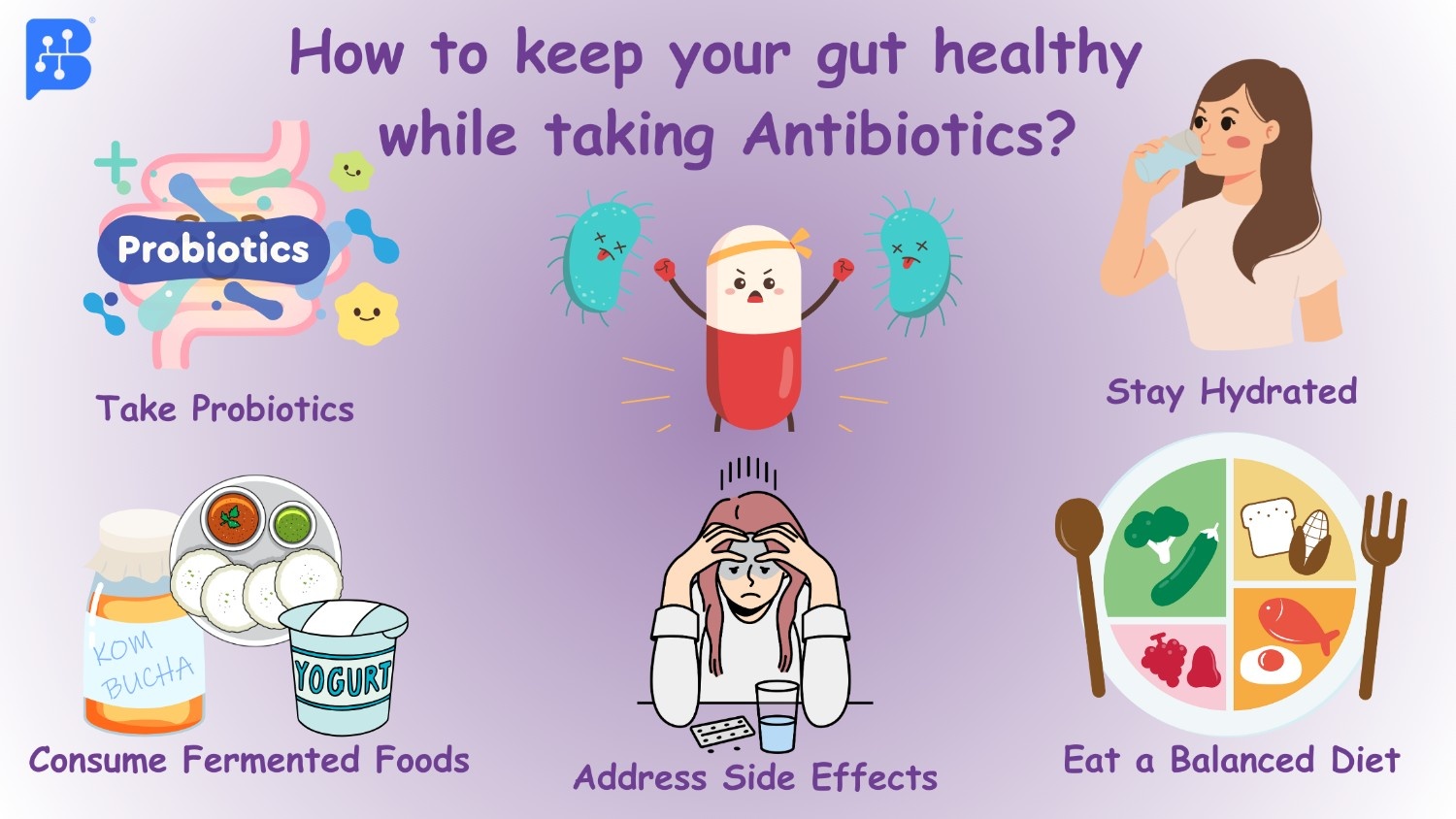
Img-1: Precautions to be taken while taking antibiotics.
When consuming antibiotics prescribed by a doctor, it is crucial to take sufficient care of your gut. You can add probiotic supplements if necessary and consume fermented foods to maintain gut health. Additionally, staying hydrated and maintaining a balanced diet are important. If any side effects of antibiotics are observed, please seek expert advice.
Maintaining a healthy gut when taking antibiotics is critical to minimizing the alteration of the gut microbiota and lowering the possibility of antibiotic-related adverse effects.
The following advice will help you maintain a healthy stomach while taking antibiotics:
Take Probiotics: Consider taking probiotic supplements containing helpful bacteria like Lactobacillus and Bifidobacterium. The good bacteria in your stomach that antibiotics may have destroyed can be restored with the use of probiotics. To make sure probiotics are safe and suitable for you, consult with your doctor before beginning any supplementation.
Consume Fermented Foods: Include foods like yoghurt, kefir, sauerkraut, kimchi, and kombucha in your diet that have undergone fermentation. Natural probiotics found in these foods can aid in maintaining a balanced population of good gut flora.
Stay Hydrated: Since antibiotics can occasionally result in dehydration, make sure you drink lots of water to stay hydrated. Drinking enough water promotes intestinal health in general and aids in the removal of toxins from the body.
Eat a Balanced Diet: Pay attention to consuming a diet high in whole grains, fruits, vegetables, lean meats, and healthy fats. Essential minerals and fiber from various foods improve intestinal health and encourage the growth of good bacteria.
Eat Less Sugary and Processed Foods: Consuming too much sugary and processed food might upset your stomach's natural balance and encourage the growth of dangerous bacteria. To support a healthy gut environment, choose whole foods that are high in nutrients instead.
Take Antibiotics as Directed: Follow your doctor's instructions for taking antibiotics exactly as prescribed. Even if you feel better before finishing the course of antibiotics, take them all to be sure the infection is completely cleared.
Address Side Effects: Talk to your doctor if you have any gastrointestinal side effects after taking antibiotics, such as nausea, diarrhoea, or upset stomach. To treat these symptoms, they could advise changing your antibiotic treatment or recommending extra medications.
Promote Digestive Health: Include foods high in prebiotic fibres, which support the growth of good gut bacteria, such as onions, garlic, bananas, asparagus, and oats. Consider using digestive enzymes or herbal supplements to support digestive function and reduce gastrointestinal discomfort.
Conclusion
In conclusion, the widespread and often indiscriminate use of antibiotics presents serious concerns despite their undeniable contributions to modern medicine. Antibiotic resistance poses a significant threat to their effectiveness in treating infections, while the collateral harm to the gut microbiota underscores the importance of responsible antibiotic use to mitigate long-term health risks. These gut modifications extend beyond immediate health concerns, affecting metabolic function and immune response. Strategies such as probiotic supplements and a balanced diet are crucial for maintaining gut health during antibiotic use. However, addressing antibiotic misuse requires coordinated efforts to promote alternative infection control methods, raise public awareness, and foster responsible antibiotic practices. By prioritizing both the therapeutic benefits of antibiotics and the preservation of gut health, we can combat antibiotic resistance and safeguard public health for future generations.
References
-
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8756738/
-
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7732679/
-
https://www.the-scientist.com/what-happens-to-the-gut-microbiome-after-taking-antibiotics-69970
-
https://www.kemin.com/in/en/blog/animal/managing-gut-health-with-antibiotic-alternatives