- Feb. 5, 2024
- Siddhi Talgaonkar
- Gestational and Neonatal
How and Why to Cultivate a Healthy Gut During Pregnancy
Pregnancy is a wonderful time in a woman's life when her body transforms into a safe haven and she writes a story about love, excitement, and the joyful birth of a tiny miracle. Every heartbeat, a gentle note creating the harmony of a fresh existence, is created with unwavering love and care as she nourishes the priceless gift inside her womb.

Ensuring the health and nutrition of mothers is critical to ensuring the survival of their babies. Poor maternal health and illnesses can significantly increase the risk of negative outcomes for newborns, including stillbirths, neonatal deaths, and other clinical complications. It becomes clear that promoting the health of moms and their infants requires an integrated approach to maternal health.
Pregnancy brings about intentional changes in the body and mind, beyond hormonal fluctuations and uterus growth; these changes facilitate women's smooth and easy transition into the complex role of motherhood on all levels-physical, emotional, and psychological.
It brings about several adaptations, such as:-
- An abrupt increase in the mother's cardiac output,
- Immunological modifications such as increased T-regulatory cells, which peak in the second trimester, and
- Modifications to the gut microbiome, which represent the dynamic changes that occur throughout her body.
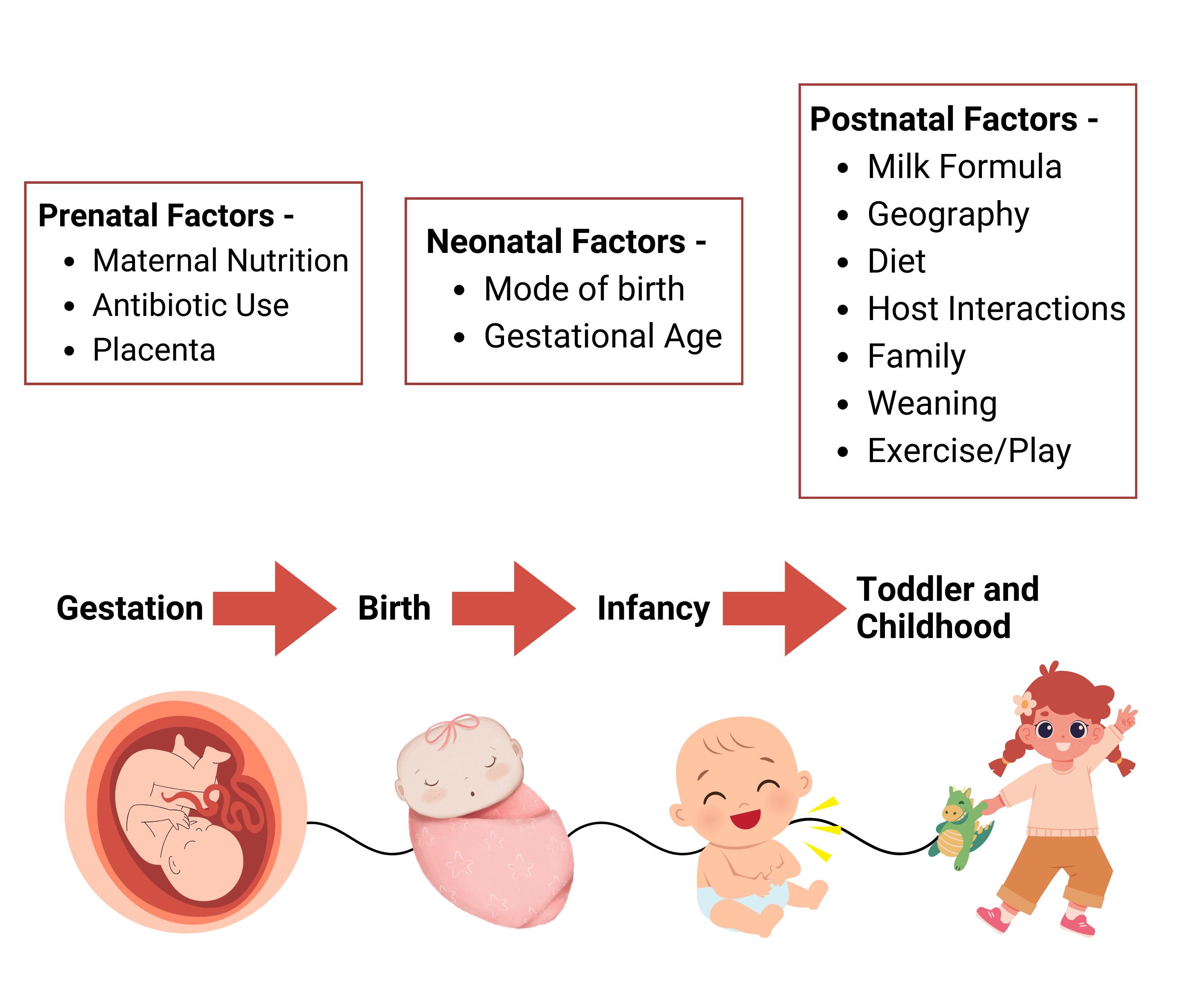
Even though the main factors that significantly shape the microbial makeup of a baby are the mode of birth, breastfeeding, and early-life antibiotic therapy, pregnancy-related maternal variables like nutrition, weight, and antibiotic use are the prenatal factors in the microbiome of the unborn child.
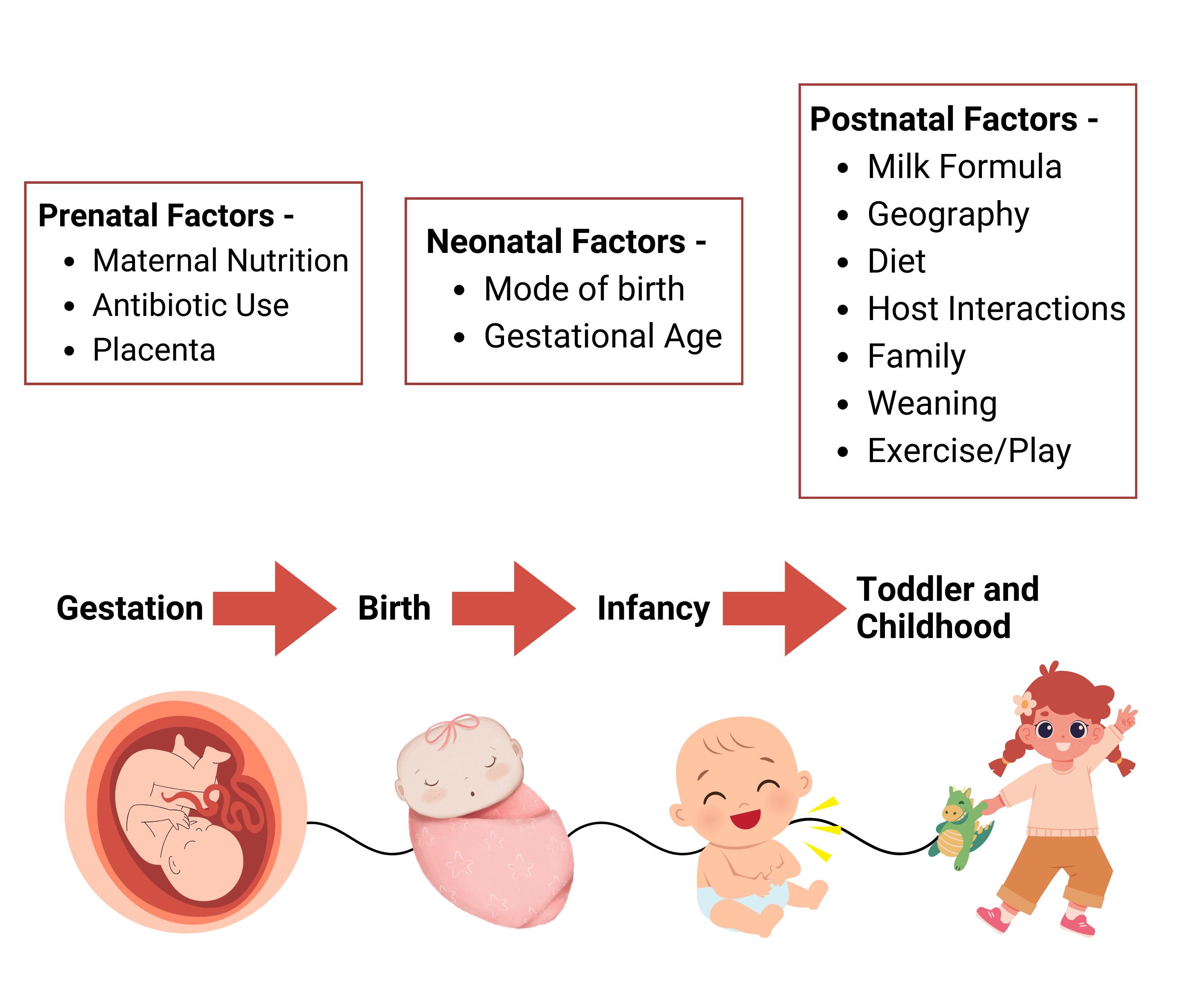
Image 1- Factors affecting gut health at different stages
The above picture depicts the different factors that affect a newborn’s microbiome. Gestation is the prenatal stage where maternal nutrition, the use of antibiotics, and the placenta affect the gut health of the baby. In the neonatal stage, the gut health of a newborn depends on the mode of birth and gestational age of the mother. Later in the postnatal stage, i.e., the childhood of the baby, multiple factors like milk, geography, diet, host interaction, family, weaning, and exercise or play shape the gut microbiome.
Changes in the gut microbiota during infancy can affect long-term risks including obesity, diabetes, and neurological diseases, as well as health outcomes like necrotizing enterocolitis in infancy, which can be impacted by maternal factors, delivery methods, and surroundings components.
The makeup of the woman's gut microbiome also has a substantial impact as a result of childbirth, with long-term health consequences for both the mother and the infant.
Let us look at some of the significant changes that occur in a mother's body while the fetus develops.
What are the changes taking place in the mother's body?
Hormonal changes
The delicate balance of hormones is essential for the successful outcome of pregnancy since they are the body's complex messengers, coordinating reactions across different tissues and organs. Many hormones alter significantly throughout pregnancy, each with a specific function.
- Human Chorionic Gonadotropin hormone (hCG), which is solely generated in the placenta, increases significantly during the first trimester (first 12 weeks), probably contributing to nausea and vomiting.
- Human Placental Lactogen (hPL) has two functions: it feeds the fetus and stimulates breast milk glands in preparation for future nursing. To maintain a healthy pregnancy, the placenta also produces estrogen, which is essential for the development of female sexual characteristics.
- Furthermore, progesterone, which is produced by the placenta and the ovaries throughout pregnancy, aids in the thickening of the uterine lining and creates an environment that is favorable for the implantation of a fertilized egg.
Significant hormonal changes throughout the first few weeks of pregnancy cause distinct immunological and inflammatory alterations that affect gut microbiota and function.
Estrogen and progesterone influence the makeup of the gut microbiome by influencing the bacterial metabolism, proliferation, and virulence of pathogenic bacteria. Gut contractility and transit are also impacted by significant ovarian hormone fluctuations that occur throughout the prenatal and postpartum phases. During pregnancy, the body may release hormones that slow down the rate at which food passes through the stomach and intestines. This might be a beneficial reaction since it gives the body more time to absorb nutrients, allowing the pregnant woman and baby to gain weight.
Metabolic changes
Pregnancy causes significant alterations in the mother's metabolism. Early gestation can be considered an anabolic condition (the building of complex molecules from numerous simple ones) in the mother, with an increase in maternal fat storage and minor changes in insulin sensitivity. As a result, nutrients conserved throughout early pregnancy fulfill the placental and maternal demands of late gestation and nursing.
Late pregnancy, on the other hand, is best characterized as a catabolic condition (involving the breakdown of complex molecules into simpler forms) with lower insulin sensitivity (increasing insulin resistance). Maternal glucose and free fatty acid concentrations rise as insulin resistance increases, providing more substrate availability for fetal development.
The microbial diversity in the gut during the commencement of pregnancy appears to be comparable to that of non-pregnant women. However, in over 70% of women, the quantity of gut bacteria linked to inflammatory conditions rises as pregnancy progresses. The ratio of specific important bacteria (Firmicutes:Bacteroidetes) in the gut microbiota changes most, resembling the increased concentrations of Firmicutes associated with obesity. Serum levels of proinflammatory cytokines (such as TNF-a, IL-2, IL-6, and IFN-y) also increase, and the mucosal surfaces of the gastrointestinal system exhibit low-grade inflammation.
Immunologic Changes
The mother's immune system undergoes significant changes throughout pregnancy to defend against infections and prevent harmful immunological reactions against the allogeneic fetus (the fetus carrying distinct genetic material from the mother or the combination of genetic material from the mother and father). While there is little evidence that the maternal immune system is universally reduced during pregnancy, elevated risks for some types of illnesses imply significant qualitative immunological alterations. A better understanding of immunological changes during pregnancy may also be essential in determining effective techniques for using vaccinations, such as influenza and pertussis, to protect both the pregnant mother and the newborn.
There are many inflammatory states throughout pregnancy, ranging from increased inflammation during implantation and labor to decreased inflammation in the middle of the pregnancy. Although the placental bed has anti-inflammatory qualities that protect the fetus from rejection, the mucosal surfaces of the intestinal tract and other tissues suffer low-grade inflammation with increased amounts of pro-inflammatory cytokines and white cells as the pregnancy progresses.
Beyond these few major modifications, women's bodies have undergone several more changes as well. Both the mother and the infant go through a lot of changes from the first day until the baby is born, which affects each differently. While most of the changes are positive for both individuals, a small number of them may increase risk or cause disease.
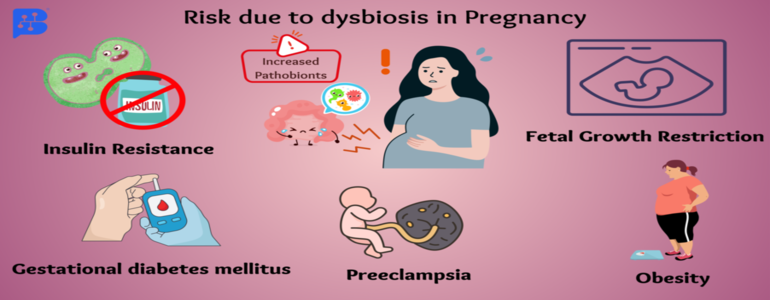
Risk of developing various ailments during pregnancy due to dysbiosis
-
The gut microbiome plays a critical role in the renewal of epithelial cells and the maintenance of intestinal integrity, which in turn affects an individual's systemic and intestinal immune systems. Bacteria go from the gut into the bloodstream when the intestinal wall is unhealthy, which worsens systemic inflammation. This movement is caused by an intestinal permeability process known as "leaky gut."
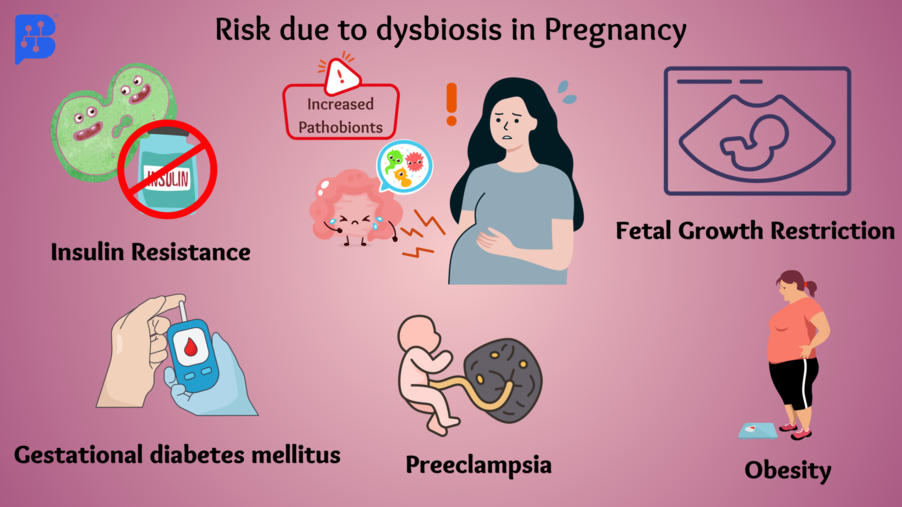
- Dysbiosis is thought to be connected to low-grade inflammatory illnesses such as obesity and related ailments, insulin resistance, and Type 2 diabetes, through increased intestinal permeability. High permeability makes it possible for bacteria to seep out and/or for bacterial components, such as the lipopolysaccharides (LPS) found in gram-negative bacteria's cell walls, to cause metabolic endotoxemia, a harmful systemic inflammatory disease.
-
Preeclampsia is a serious problem in obstetrics, affecting 2-8% of pregnancies globally. It is among the most frequent reasons for morbidity and death among expectant women and their children throughout the perinatal stage. Preeclampsia's process is still not entirely understood. Researchers discovered that the abnormal shape of the placenta might harm blood vessels, resulting in preeclampsia during pregnancy. Preeclampsia may be associated with metabolic syndrome, a disorder characterized by impaired glucose and lipid metabolism, insulin resistance, and damage to the blood vessel lining.
- Some research suggests a relationship between preeclampsia and the mother's gut flora, with decreased levels of particular beneficial bacteria like Prevotella, Porphyromonas, Varibaculum, and Lactobacillus in women with preeclampsia. Prevotella is a multipurpose bacteria found in the human digestive system. It acts as a defense against microbial illnesses.
-
Fetal Growth Restriction (FGR), also known as Intrauterine Growth Restriction (IUGR), is a common pregnancy issue. It happens when the baby doesn't grow properly in the womb due to reasons like infections, advanced maternal age, malnourishment, genetic problems, or a placenta that can't provide enough nutrients.
- Some studies suggest a potential link between the gut bacteria (microbiota) and FGR. In one study of 6,000 pregnant women, Helicobacter pylori was connected to FGR.
- Stool samples from pregnant women with FGR showed differences in the proliferation of Bacteroides, Faecalibacterium, and Lachnospira compared to a control group, indicating a possible role of gut bacteria in FGR.
-
In addition to increasing the risk of obesity, type 2 diabetes, and metabolic syndrome, gestational diabetes mellitus (GDM) is the most prevalent metabolic consequence of pregnancy. Blood glucose levels are impacted by metabolic changes that are mediated by the gut bacteria. For many experts, the question of whether intestinal dysbiosis contributes to the development of GDM remains controversial.
- As the pregnancy proceeds, the kinds of bacteria in the stomach change, particularly in the middle and late stages. Research on Gestational Diabetes Mellitus (GDM) discovered that people with GDM had more of a kind of bacteria called Firmicutes and fewer of another type called Bacteroidetes. In addition, in the third trimester of pregnancy, persons with GDM had a larger ratio of Firmicutes to Bacteroidetes (F/B) than those without.
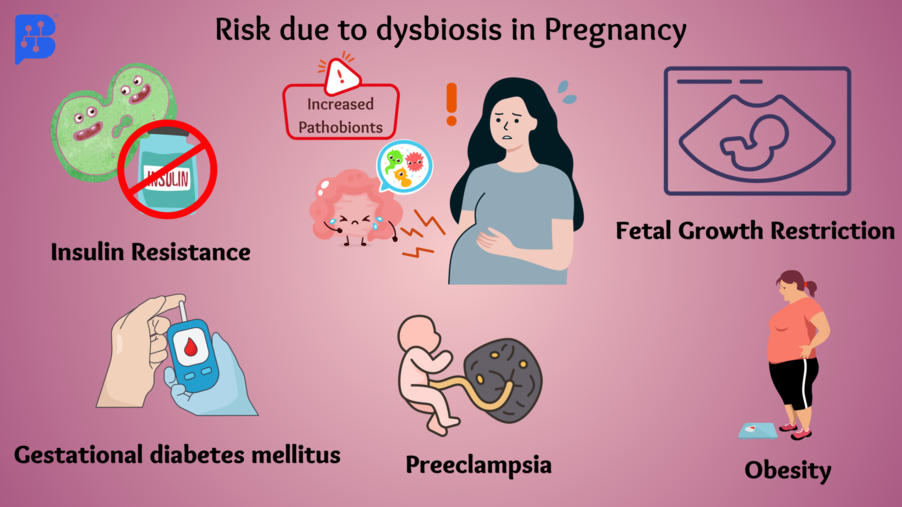
Image 2- Major risk in pregnancy due toincreased pathobionts
The above images tell us about risky conditions for pregnant ladies when there is an increase in pathobionts. Pathobionts are microorganisms such as bacteria, viruses, or fungi that are normally found in the human microbiome but can become pathogenic in particular situations. Insulin resistance, gestational diabetes mellitus, preeclampsia, obesity, and fetal growth restriction are some of the commonly observed risks during dysbiosis.
Preventive measures to be taken for a healthier baby's gut
-
Increase your intake of prebiotic foods, including bananas, oats, onions, asparagus, legumes, etc. Additionally, meals containing chemicals, artificial sweeteners, and food colors are bad for your gut health since they interact with probiotics.
-
Reduce your coffee intake in the late afternoon and make time for restful sleep. Establish a nightly routine that communicates to your body when it's time to relax and regenerate. Additionally, try to go to bed and wake up at the same time every day. These techniques, commonly called "sleep hygiene," have a beneficial effect on weariness and stress.
-
Lower your stress levels by engaging in regular exercise, deep breathing, and meditation. It seems to make sense that pregnant women may feel a stronger desire to remain still. Some tend to induce constant sleepiness. While these changes are to be expected, remaining active is crucial for your health and that of the developing fetus.
- Pregnancy-related exercise may have a positive prenatal impact, fostering a healthy environment in the womb during a crucial stage of organ development. The benefits to offspring can be observed in terms of body weight and composition, cardiovascular health, and nervous system development.
- Women can adopt healthy lifestyle practices that can improve postnatal health and lower their child's chance of acquiring chronic illnesses, including obesity, diabetes, and cardiovascular disease (CVD).
- Exercise is excellent for both mental and physical health, and it also improves gut health by lowering inflammation and changing the way the body is built.
- Exercise also encourages favorable alterations in the makeup of the gut microbiota that are created in the gastrointestinal system.
- It’s believed that exercise during pregnancy can lead to larger placentas, providing the fetus with more oxygen and nutrients.
- It’s important to remember that everyone is unique and needs individualized care. The key is to maintain physical activity through exercises that are gentle and that your body is familiar with.

Image 3- A few things to remember during pregnancy
The above picture talks about some important reminders for the pregnant lady. It is very important to follow a healthy diet routine and avoid processed foods. Daily exercise, meditation, and mindful activities are also necessary to live a happy and peaceful life. Have a good 6-7 hours of sleep and follow up with regular checkups..
Conclusion
In conclusion, a woman's body undergoes a symphony of changes throughout pregnancy, including modifications to her metabolism, major immunological changes, and hormonal shifts, all intricately linked to the health of both mother and child. The gut microbiome emerges as a pivotal player, influencing long-term health implications. The potential influence of the gut microbiota on maternal and fetal health is highlighted by the connections between dysbiosis and diseases such as gestational diabetes mellitus, fetal growth restriction, and preeclampsia. As we navigate these transformations, embracing preventive measures such as a balanced diet, adequate sleep, stress reduction, and mindful activities becomes paramount. By nurturing gut health during pregnancy, we not only promote a smoother journey into motherhood but also contribute to the well-being of generations to come.
So, dear ladies, as you embark on the adventure of motherhood or intend to bring a new life into the world, are you ready to protect not only your health but also that of the precious life growing inside of you by nurturing your gut health?
References
1. Lothian, J. A. (2008). The journey of becoming a mother. The Journal of perinatal education, 17(4), 43-47.
2. Edwards, S. M., Cunningham, S. A., Dunlop, A. L., & Corwin, E. J. (2017). The maternal gut microbiome during pregnancy. MCN. The American journal of maternal child nursing, 42(6), 310.
3. Gorczyca, K., Obuchowska, A., Kimber-Trojnar, Z., Wierzchowska-Opoka, M., & Leszczynska-Gorzelak, B. (2022). Changes in the gut microbiome and pathologies in pregnancy. International journal of environmental research and public health, 19(16), 9961.
4. Yao, Y., Cai, X., Chen, C., Fang, H., Zhao, Y., Fei, W., ... & Zheng, C. (2020). The role of microbiomes in pregnant women and offspring: research progress of recent years. Frontiers in Pharmacology, 11, 643.
5. Lain, K. Y., & Catalano, P. M. (2007). Metabolic changes in pregnancy. Clinical obstetrics and gynecology, 50(4), 938-948.
6. Abu-Raya, B., Michalski, C., Sadarangani, M., & Lavoie, P. M. (2020). Maternal immunological adaptation during normal pregnancy. Frontiers in immunology, 2627.
7.https://www.niddk.nih.gov/health-information/weight-management/healthy-eating-physical-activity-for-life/health-tips-for-pregnant-women