The Hidden Dangers of an Imbalanced Gut Microbiome
Introduction
The human microbiome is made up of a vast array of microbes including bacteria, archaea, virus and eukaryotes with a prominent number of bacteria residing in the gastrointestinal tract. It is estimated that the human body harbor approximately 10^13 to 10^14 microbial cells that play a significant role in regulating host metabolic and physiological processes.
Recent advancements in sequencing technologies and large-scale projects like the Human Microbiome Project (HMP) have significantly enhanced our understanding of the microbiome's composition and function. These projects have utilized techniques such as 16S rRNA sequencing and Whole Genome Shotgun (WGS) metagenomic sequencing to characterize microbial communities.
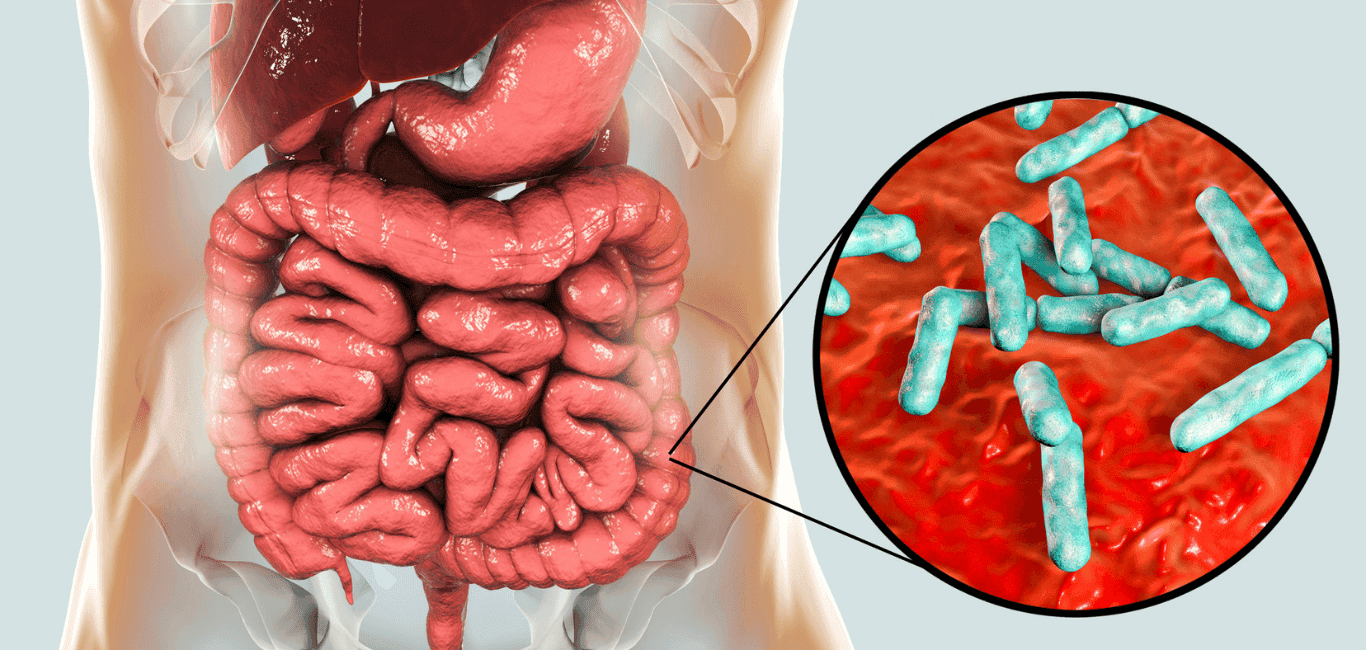
Gut microbiome and its functions
The gut microbiome plays a crucial role in maintaining overall health by interacting with the host through several immune, metabolic and neuroendocrine pathways. The metabolites produced by gut microbes serve as signaling molecules that facilitate communication between the gut and other organ systems. Another prominent function of the gut microbiota is to help in breakdown of the dietary fibres into short chain fatty acids (SCFA’s) that regulate several immune and inflammatory responses. Apart from detoxifying complex molecules, beneficial gut bacteria also secrete metabolites that support colon health, manage tissue inflammation, and improve digestion of fats.
Microbial dysbiosis and diseases
As gut microbiome research moves forward, there is more scientific data that explains the link between gut dysbiosis and overall well-being of an individual. Gut dysbiosis can result from several factors like overuse of antibiotics, dietary patterns, environmental changes and stress, thus impairing gut function and can lead to secretion of harmful microbial products, contributing to various diseases.
Several studies explain how microbial imbalances are associated with conditions like IBD, obesity, diabetes, cardiac health, mental health and neurological disorders. Let us discuss here about a few major implications of an imbalanced gut microbiome.
Increased inflammation:
Gut dysbiosis frequently causes immune cells to become hyperactivated, impairing immunological responses and causing chronic inflammation and damage to the gut lining. This chronic inflammation leads to a number of diseases, including IBD.
Gastrointestinal disorders:
An imbalanced gut is linked to improper functioning of the GI tract with symptoms ranging from bloating, abdominal pain and diarrhoea.
Autoimmune diseases:
Dysbiosis can contribute to the development of autoimmune disorders like celiac disease. The increased count of pro- inflammatory gut bacteria disrupts the intestinal membrane integrity, causing a condition known as ‘leaky gut’ in which toxic substances re-enter the bloodstream triggering autoimmune responses.
Metabolic disorders:
An unhealthy gut impairs metabolic functioning. According to research, the gut microbiota is crucial for the digestion and absorption of food, and when this process is disrupted, weight gain and insulin resistance result, which can lead to metabolic disorders including obesity.
Mental health issues:
There is increasing evidence that suggests that gut health is linked to our mental wellbeing. Gut dysbiosis results in impaired secretion of neurotransmitters and metabolites that lead to altered gut-brain axis communication resulting in several mood disorders, depression and anxiety.
Increased risk of cancer:
Studies reveal certain metabolites produced by an imbalanced gut microbiome promotes carcinogenesis through DNA damage and chronic inflammation. For example, a reduction in the number of beneficial butyrate producing gut bacteria has been associated with colorectal cancer, as butyrate has a protective effect against tumor development.
Cardiovascular diseases (CVD):
In an imbalanced gut, the gut bacteria often convert the dietary choline into trimethylamine N-oxide (TMAO) that hardens the arteries and promotes plaque build-up leading to cardiovascular diseases.
Osteoporosis:
Inflammatory molecules that promote bone deterioration are released more frequently by an imbalanced gut. Additionally, lower SCFA levels encourage worse bone health and calcium absorption.
Simple ways to fix these gut imbalances
Maintaining gut health is a multifactorial process in which gut imbalances can be restored over time by following certain targeted interventions such as change in dietary patterns, sleep cycle regulation, regular physical activity and better stress management.
Following healthy dietary patterns has been one of the effective ways to restore beneficial gut bacteria as the food we eat impacts the gut microbiome composition and diversity. Consuming fibre rich foods like oats, fruits, vegetables, and whole grains helps in better food digestion, maintain gut membrane integrity and enhance microbial diversity. Additionally consuming fermented foods like idli, dosa, yogurt that are rich in healthy bacteria promote better gut health and reduce tissue inflammation. Likewise, one also needs to reduce the intake of processed foods and excess sugars to prevent growth of harmful bacteria that promote gut dysbiosis.
Supplementing with both probiotics (live beneficial bacteria) and prebiotics (nondigestible food components that promote growth of beneficial gut bacteria) can also help to restore gut imbalances. The most commonly used probiotic microorganisms are- Lactobacillus, Bifidobacterium and Saccharomyces boulardii.
Road to the future- Human Gut microbiome research
Personalised medicine- Deciphering the unique composition of an individual’s gut microbiome can pave way for personalised treatment plans. By analysing the microbiota composition, health care providers can tailor interventions such as probiotics or dietary recommendations that could restore gut imbalances. Microbiome analysis may also help to analyse an individual's drug responses as differences in the gut microbiota composition can impact how an individual responds to any drug or therapy. Advancing research in this direction can shift the one size fits all approach to precision healthcare based on gut microbial signature sequences.
Preventive care- Monitoring and managing gut health could play a crucial role in alleviating symptoms associated with several inflammatory conditions like IBD and obesity. These probiotics can be used as adjunct therapies in disease management.
Novel therapeutics-Microbial based therapeutics such as fecal microbial transplantation (FMT) and genetically modified probiotics open up new avenues for patients suffering from dysbiosis related diseases who do not recover with conventional treatments.
As microbiome-based therapies become more prevalent, regulatory bodies may need to establish guidelines for the safety and efficacy of probiotics and other microbiome-modulating treatments. Ensuring that these products are safe for public use is essential for their acceptance and integration into healthcare systems.