Anxiety is a mental health condition characterized by excessive, persistent worry, fear, or nervousness that is intense enough to interfere with daily activities and functioning. It remains one of the most understated mental health conditions in India, often overlooked due to limited awareness among parents, teachers, and even healthcare providers. Social stigma, lack of education around mental health, and the tendency to dismiss emotional struggles as mere “stress” or “overthinking” further contribute to underdiagnosis and inadequate support. As a result, many individuals, especially young people suffer in silence without the tools or understanding needed to seek help. But emerging science shows that it is not as much of a "it's all in your head” problem as we think it is.
Anxiety in India: What the Data Says
The National Mental Health Survey (NHMS) was last conducted in 2015–16 in India. It was found that 3.5% of the population was dealing with some form of stress or anxiety-related disorder. This might sound like a small number, but it adds up to over 40 million people across the country.
The survey showed that anxiety was most common among young adults aged between 18 to 29 years and affected women compared to men. It was also observed that anxiety was more prevalent in urban areas than the rural ones.
Generalised Anxiety Disorder (GAD) is more than just feeling stressed .It is accompanied by symptoms like constant worry, restlessness, fatigue, and trouble concentrating, all of which can interfere with day-to-day activities. Although various treatment options, including medications and therapies, are available, managing the symptoms of Generalized Anxiety Disorder (GAD) can still be challenging.
Common medications for Generalized Anxiety Disorder (GAD) include antidepressants like fluoxetine (Prozac) and sertraline (Zoloft). These drugs work by increasing the availability of serotonin, a “feel-good” hormone that helps to regulate mood and reduce anxiety. Even though they are considered standard medications, continued usage might require higher doses to have the same effect. Along with dose-dependent tolerance, side effects of these anxiolytic drugs (anti-anxiety drugs) include nausea, diarrhoea, dizziness, and headaches.
Despite anxiety being the most prevalent mental health condition, there has been limited research on development of anxiolytic drugs with the aim of better treatment outcomes and fewer side effects.
In this regard, attempts have been made to develop alternative approaches for the treatment or alleviation of symptoms of mental health conditions like anxiety disorders. Research has shown that the gut microbiome has a major role in physical as well as mental health. This has given rise to a concept of ‘psychobiotics’- probiotics for improvement of mental health, as a potential treatment for various mental health conditions and in alleviation of symptoms associated with anxiety.
The connection between the gut and mind
What does it mean when we say the gut is connected to the mind?
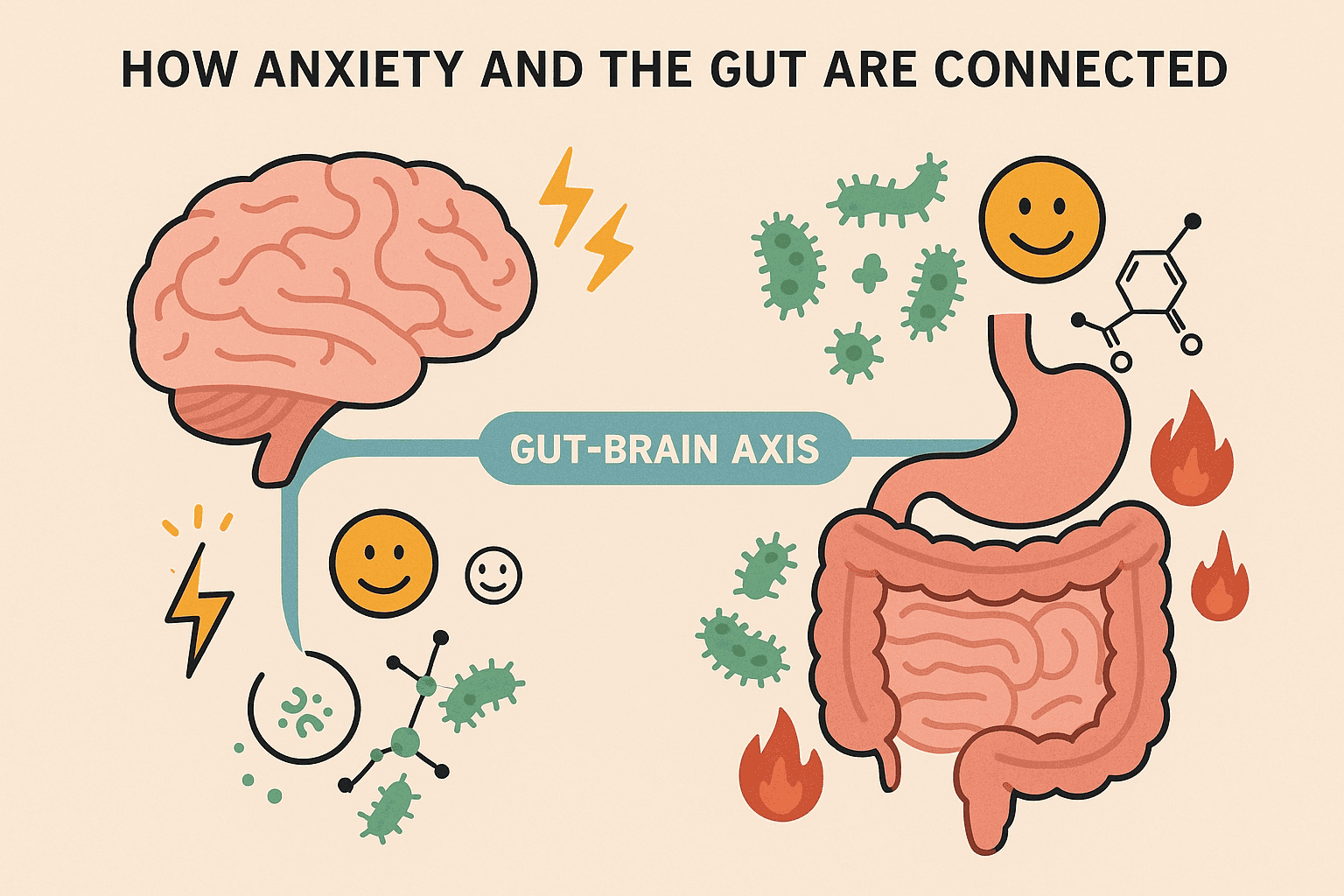
When people say the gut is linked to the mind, they’re referring to something called the gut-brain axis. This is a two-way communication system between your gut and your brain. The main messenger in this system is the vagus nerve, carrying signals back and forth.
A key player in this connection is the gut microbiota, the trillions of bacteria living in your digestive tract. Some of the key gut microbial genera like Bifidobacterium and Lactobacillus are now known to help to keep both your gut and brain in good shape. They do this by producing important chemicals called neurotransmitters, like serotonin and Gamma-aminobutyric acid (GABA), which are often called "feel-good" chemicals because they help regulate mood and anxiety. In fact, lots of neurotransmitters are produced by the gut itself- 90% of the body's serotonin is actually produced by Enterochromaffin (EC) cells in the gut lining.
Another way these bacteria influence the gut-brain axis is through their ability to break down dietary fiber into short-chain fatty acids (SCFAs). These molecules are essential for energy production, reducing inflammation, maintaining blood sugar balance, and preserving the integrity of the gut lining. Beyond these numerous systemic benefits, recent research indicates that SCFAs may play an important role in the gut-brain axis communication, directly impacting neurological and behavioural processes.
Several studies suggest an imbalance in the gut ecosystem of patients with anxiety. This imbalance may lead to increased inflammation, reduced production of calming neurotransmitters, and a less effective gut-brain communication system, all of which can heighten feelings of anxiousness. Evidence indicates that the abundance of Bacteroides and Escherichia-Shigella is higher in patients exhibiting anxiety symptoms. Conversely, there is a decline in the abundance of short-chain fatty acid (SCFA) producers such as Faecalibacterium, Eubacterium rectale, Lachnospira, Butyricicoccus, and Sutterella. These changes in gut microbiome composition may contribute to the worsening of anxiety symptoms.
How can we implement this information to improve our anxiety symptoms?
It is becoming increasingly clear that we need to rethink how we approach mental health conditions like Generalized Anxiety Disorder (GAD) and other anxiety-related disorders.
Traditionally, these conditions have been viewed primarily through a psychological lens, often separate from physical health. However, growing evidence suggests that mental health and physical health are deeply interconnected, particularly through systems like the gut-brain axis. Multiple studies show that the presence or absence of the gut microbiota plays a very important role in mood related disorders. This evolving understanding calls for a more holistic approach; one that gives mental health the same level of attention, care, and legitimacy as physical illnesses.
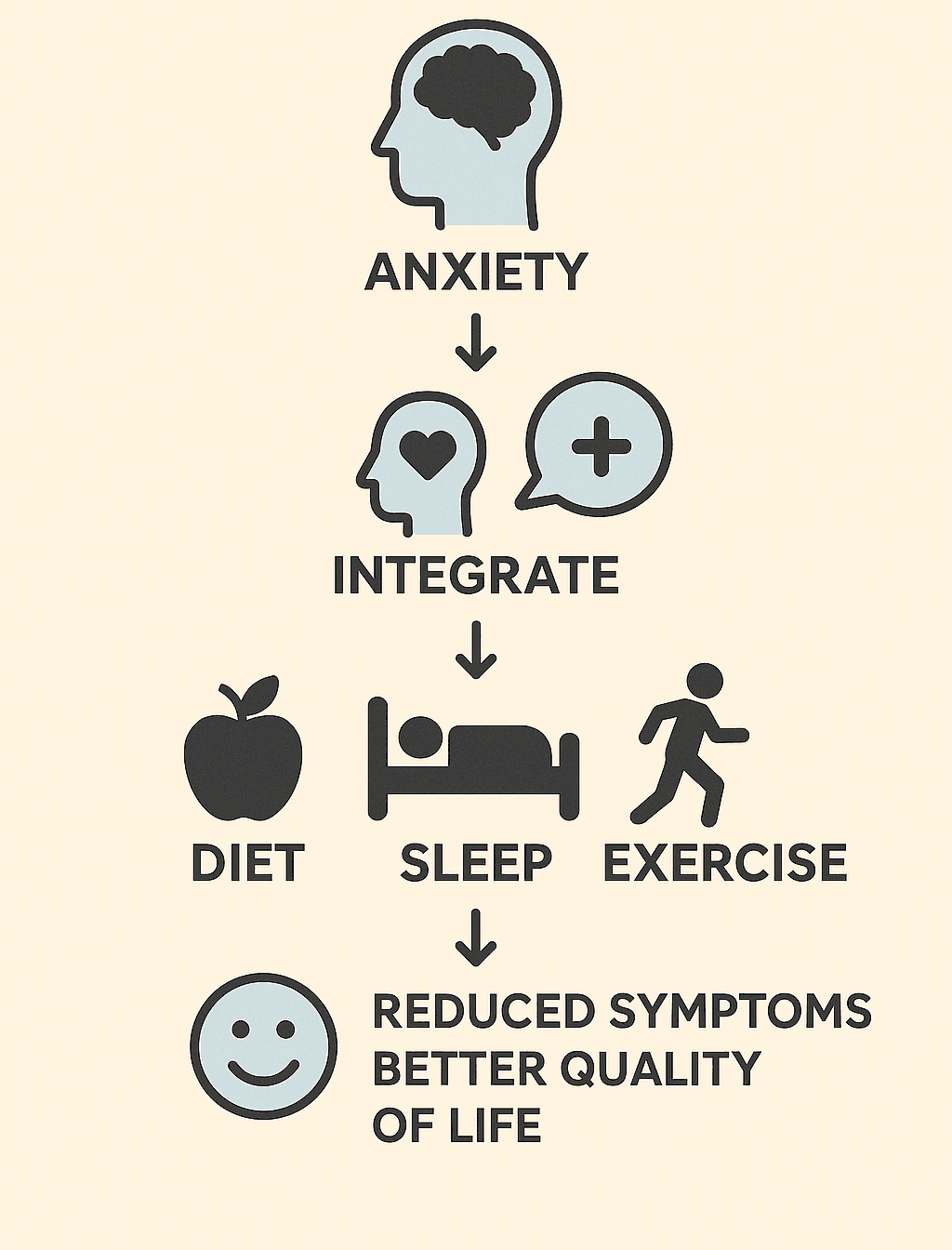
Recognizing anxiety disorders as conditions that may have biological, physiological, and lifestyle-related underpinnings opens the door to new avenues for treatment and management. By shifting our perspective, we can begin to explore the role of diet, exercise, sleep, and gut health as part of a broader strategy for improving mental well-being. Simple, everyday changes such as incorporating nutrient-dense foods, prioritizing gut-friendly meals, practicing stress-busting hobbies, and maintaining consistent routines can play a meaningful role in alleviating symptoms and supporting long-term mental health. Research also now shows that supplementation with probiotics like Lactobacillus and Bifidobacterium (the "psychobiotics mentioned earlier!) can even reduce the severity of anxiety symptoms, and this could support other gut-healthy practices in boosting relief.
An integrative approach has the potential not only to improve quality of life but also to reduce the stigma often associated with mental illness, by framing it as a comprehensive health issue deserving of multifaceted solutions.
Foods to boost the gut-brain connection
Eating the right foods and maintaining a consistent meal schedule might sound like basic, even cliché advice, but these habits have a far greater impact than they appear to at first glance. What seems like a minor lifestyle tweak can actually lead to profound improvements in physical and mental well-being. While it may feel unnecessary or easy to overlook, giving mindful eating a genuine try can yield noticeable benefits.
Here are some foods to improve the symptoms of anxiety:
Good fats like ghee, butter, olive oil, butter
Fermented foods like sauerkraut, kimchi, yogurt, kefir
High-quality animal protein like eggs, grass-fed meats, pastured poultry, organ meats (like liver), fish (especially oily fish like salmon, sardines, and mackerel)
Broths (bone broths rich in minerals and collagen)
Sprouts, sea vegetables, miso, and apple cider vinegar
Complex carbs, such as sweet potato, squash
Avoid excessive sugar and ultra-processed foods, which can disrupt gut bacteria. Limit alcohol and caffeine, which can irritate the gut and exacerbate anxiety. Aim for a variety of diverse plant foods that feed a more diverse microbiome.
Anxiety can be difficult to manage but you can give it your best to try to manage or eliminate the symptoms. This is not medical advice but just a new holistic way to approach mental health problems. Please consult a therapist for severe symptoms. You are not alone in this. Help is available.
-Navya Aghariya
References
- Manjunatha, N., Jayasankar, P., Suhas, S., Rao, G. N., Gopalkrishna, G., Varghese, M., Benegal, V., & NMHS National Collaborators Group (2022). Prevalence and its correlates of anxiety disorders from India's National Mental Health Survey 2016. Indian journal of psychiatry, 64(2), 138–142. https://doi.org/10.4103/indianjpsychiatry.indianjpsychiatry_964_21
- Barrera, T. L., & Norton, P. J. (2009). Quality of life impairment in generalized anxiety disorder, social phobia, and panic disorder. Journal of anxiety disorders, 23(8), 1086–1090. https://doi.org/10.1016/j.janxdis.2009.07.011
- Strawn, J. R., Geracioti, L., Rajdev, N., Clemenza, K., & Levine, A. (2018). Pharmacotherapy for generalized anxiety disorder in adult and pediatric patients: an evidence-based treatment review. Expert opinion on pharmacotherapy, 19(10), 1057–1070. https://doi.org/10.1080/14656566.2018.1491966
- Garakani, A., Murrough, J. W., Freire, R. C., Thom, R. P., Larkin, K., Buono, F. D., & Iosifescu, D. V. (2021). Pharmacotherapy of Anxiety Disorders: Current and Emerging Treatment Options. Focus (American Psychiatric Publishing), 19(2), 222–242. https://doi.org/10.1176/appi.focus.19203
- Chen, Y. H., Bai, J., Wu, D., Yu, S. F., Qiang, X. L., Bai, H., Wang, H. N., & Peng, Z. W. (2019). Association between fecal microbiota and generalized anxiety disorder: Severity and early treatment response. Journal of affective disorders, 259, 56–66. https://doi.org/10.1016/j.jad.2019.08.014
- Bravo, J. A., Forsythe, P., Chew, M. V., Escaravage, E., Savignac, H. M., Dinan, T. G., Bienenstock, J., & Cryan, J. F. (2011). Ingestion of Lactobacillus strain regulates emotional behavior and central GABA receptor expression in a mouse via the vagus nerve. Proceedings of the National Academy of Sciences of the United States of America, 108(38), 16050–16055. https://doi.org/10.1073/pnas.1102999108
- Aslam, H., Green, J., Jacka, F. N., Collier, F., Berk, M., Pasco, J., & Dawson, S. L. (2020). Fermented foods, the gut and mental health: a mechanistic overview with implications for depression and anxiety. Nutritional neuroscience, 23(9), 659–671. https://doi.org/10.1080/1028415X.2018.1544332
- Ferrari, S., Mulè, S., Parini, F., Galla, R., Ruga, S., Rosso, G., Brovero, A., Molinari, C., & Uberti, F. (2024). The influence of the gut-brain axis on anxiety and depression: A review of the literature on the use of probiotics. Journal of traditional and complementary medicine, 14(3), 237–255. https://doi.org/10.1016/j.jtcme.2024.03.011
- Foster, J. A., & McVey Neufeld, K. A. (2013). Gut-brain axis: how the microbiome influences anxiety and depression. Trends in neurosciences, 36(5), 305–312. https://doi.org/10.1016/j.tins.2013.01.005
- Margoob, M., Kouser, S., & Jan, N. (2024). Serotonin: The Link between Gut Microbiome and Brain. IntechOpen. doi: 10.5772/intechopen.1003826
- Jiang, H. Y., Zhang, X., Yu, Z. H., Zhang, Z., Deng, M., Zhao, J. H., & Ruan, B. (2018). Altered gut microbiota profile in patients with generalized anxiety disorder. Journal of psychiatric research, 104, 130–136. https://doi.org/10.1016/j.jpsychires.2018.07.007
- Silva, Y. P., Bernardi, A., & Frozza, R. L. (2020). The Role of Short-Chain Fatty Acids From Gut Microbiota in Gut-Brain Communication. Frontiers in endocrinology, 11, 25. https://doi.org/10.3389/fendo.2020.00025
- Scott, T. (2011). The antianxiety food solution: How the foods you eat can help you calm your anxious mind, improve your mood, and end cravings. New Harbinger Publications.