Introduction: More Than Just a Gut Feeling
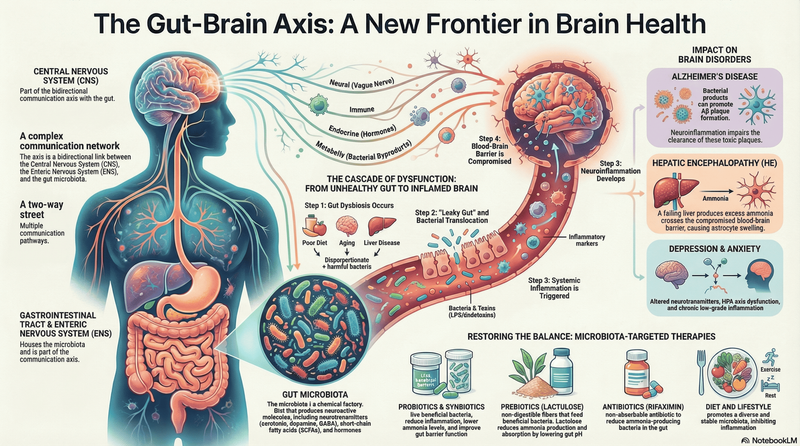
We’ve all experienced a "gut feeling" or felt "butterflies in our stomach." These common phrases are more than just metaphors; they hint at a deep, biological superhighway connecting our digestive system and our brain. Scientists call this the gut-brain axis, a complex, bidirectional communication system that links the emotional and cognitive centers of the brain with our intestinal functions. This constant dialogue involves the central nervous system and the enteric nervous system; the intricate network of neurons embedded in the walls of our gut. But this conversation isn't a private one. The gut is home to trillions of microbes that heavily influence this communication. This bustling inner ecosystem, known as the gut microbiome, doesn't just help digest food—it actively participates in shaping our mood, stress responses, and even the very structure of our brain. Here are five surprising ways your gut is influencing your mind.
1. Your Gut Is a Surprising Neurotransmitter Factory
For centuries, we've located our feelings squarely in the brain. But groundbreaking research reveals that our gut is running a parallel—and powerful—neurochemical factory of its own. Gut microbiota can produce a range of neuroactive molecules, including serotonin, GABA (gamma-aminobutyric acid), dopamine, and histamine—the very same chemicals that regulate cognition and emotion in the brain. In fact, the gut microbiome acts much like an "endocrine organ," directly producing hormones and neurotransmitters that can influence the body's overall chemistry. This means the gut isn't just sending simple status updates to the brain; it's manufacturing the very molecules the brain uses to process emotions and thoughts. This discovery challenges the conventional view that the brain is the exclusive source of our moods, suggesting that the health of our gut environment—fueled by the nutrients in our diet—plays a direct and powerful role in our mental and emotional state. This internal pharmacy isn't just for show; its output is so critical that when the microbial "pharmacists" are out of balance, the consequences can be seen directly in our mental health.
2. The Link Between Gut Bacteria and Mental Health Is Real
A growing body of scientific evidence now connects the composition of the gut microbiome to mental and neuropsychiatric health. Studies have identified dysregulation—or imbalance—of gut microbiota in conditions such as depression, anxiety, autism, and schizophrenia. The connection is so strong that researchers have demonstrated it in controlled laboratory settings. In one striking study, when germ-free rats were colonized with fecal matter from patients with major depression, the animals began to exhibit depressive-like symptoms. This finding opens up entirely new therapeutic possibilities for mental health. It suggests that interventions targeting the gut, such as specialized probiotics sometimes called 'psychobiotics,' could one day complement traditional brain-focused treatments, offering a powerful new tool for managing mental well-being. While we've seen how the gut can influence the brain, this highway runs both ways. In fact, the brain's response to stress can launch a direct assault on the very microbiome that helps regulate our mood.
3. Stress Isn't Just in Your Head—It's Remapping Your Microbiome
The effects of psychological and physical stress are not confined to the mind; they create a powerful ripple effect that directly impacts the gut environment. When you experience stress, your body activates the hypothalamus-pituitary-adrenal (HPA) axis, the central stress response system. This releases a cascade of stress hormones that can alter the composition and function of your gut microbiota. A study in a murine model, for example, found that exercise-induced stress specifically decreased levels of Turicibacter spp and increased Ruminococcus gnavus , two types of bacteria involved in intestinal function. This connection helps explain why periods of high stress often manifest as gastrointestinal distress, from stomach aches to changes in bowel habits. It reinforces the idea that stress is a whole-body phenomenon, proving that what happens in your head doesn't stay in your head—it travels down the biological superhighway and remodels your inner world.
4. Your Gut Flora Can Literally Shape Your Brain’s Immune System
The gut-brain connection is so profound that it influences the brain's fundamental cellular structure and defense systems. The brain has its own resident immune cells called microglia—its vigilant security guards, crucial for maintaining brain health and defending against injury and pathogens. Remarkably, the proper development of these cells depends on signals from our gut. Studies have shown that germ-free mice, which are raised without any gut microbiota, have immature and malformed microglia. The key to their healthy maturation appears to be short-chain fatty acids (SCFAs)—metabolites produced by gut bacteria when they break down dietary fiber. These SCFAs are critical for regulating the maturation and function of the brain's essential immune cells. This finding is profound: the health of your brain's dedicated immune patrol is directly dependent on how well you feed your gut bacteria. The fiber in your diet isn't just for digestion—it's raw material for building a resilient brain.
5. It’s Not Just About H. pylori —Your Nerves Are a Key Player in Ulcers
For decades, the bacterium Helicobacter pylori has been recognized as the primary risk factor for peptic ulcers. However, the story is more complex than a single microbial culprit. Two counter-intuitive facts challenge this simple narrative: only 10-15% of people infected with H. pylori actually develop dyspeptic symptoms, and some people develop peptic ulcers even without an H. pylori infection. So if the bacteria aren't the whole story, what is the missing piece of the puzzle? Emerging evidence points to a "nervous system imbalance, as an indispensable cofactor" in the development of gastritis and ulcer disease. This means the gut-brain axis is a critical, though indirect, player. "Although Helicobacter pylori infection is a primary risk factor for peptic ulcers, the fact that not all infected patients develop them suggests a role for other factors. Evidence points to nervous system imbalance as an indispensable cofactor, implying that the brain-gut axis plays a crucial indirect role in the disease's pathogenesis. "This insight is important because it illustrates that complex diseases are rarely caused by a single factor. It brings the age-old concept of the mind-body connection into sharp, modern scientific focus, showing how our nervous system can influence our susceptibility to diseases traditionally viewed as purely microbial.

Conclusion: The Future of Health is in Your Gut
The evidence is clear: the gut is far more than a simple digestive organ. It is a complex and dynamic ecosystem that profoundly influences our brain, mood, immune system, and overall health. The constant chemical and neural conversation happening on the biological superhighway between our gut, its resident microbes, and our brain is one of the most exciting frontiers in medical science. As researchers continue to unravel the secrets of our 'second brain,' could personalized nutrition and targeted probiotics become a frontline strategy for managing our mental and neurological well-being?
Also Read: Anxiety isn’t all in your head, it’s also in your gut !