- July 17, 2020
- BugSpeaks
- Microbiome and Disease
Being Chubby - Mark of Affluence or Aberration?
Once upon a time, being chubby and obese was a mark of affluence. As in earlier times, food was often insufficient, and famines were common obesity meant prosperity. But the world changed, and food became abundant in many regions of the world. So, what was once a mark of prosperity, has now become a sign of an unhealthy lifestyle. Obesity involves the accumulation of a considerable amount of body fat, which intensifies the risk of additional health hazards—for example, diabetes, heart disorders, liver diseases, high blood pressure, and certain cancers.
Yet, over the past few decades, obesity and related co-morbidities have reached epidemic magnitudes. People continue to eat more. The modern industrial world considers it a crisis of communal wellbeing. Generally, obesity is a result of an amalgamation of a few factors like heredity, lifestyle, and environment. Among the environmental elements, the gut microbiome flourishing in our bodies seems to play a vital role.

Our gut microbiome
As our gut plays home to a vast and diverse array of microorganisms, they, in return, play an essential role in several vital processes, like, digestion, metabolism, and energy production. Five bacteria, Bacteroidetes, Firmicutes, Actinobacteria, Proteobacteria, and Verrucomicrobia, are predominant in the gut flora of an average healthy individual, with Bacteroidetes and Firmicutes, making around 90% of the total. Our gut flora, while regulating numerous bodily processes, also influences the production, metabolism, storage, and breakdown of lipids. Lipids are the small molecules that also makeup fat.
How microscopic gut microbes influence macroscopic bodyweight?
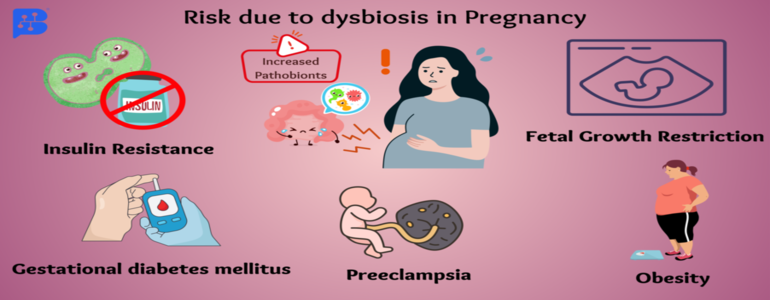
Like in other metabolic diseases, the gut microbiota in over-weight people shows misbalance as compared to normal healthy individuals. Dysbiosis, the imbalance in the proportion of good and bad gut microbes, causes varied digestion of otherwise indigestible complex carbohydrates. Such digestion of carbohydrates contributes to the risk of developing obesity.
Digestive juice of the upper GI tract cannot digest complex dietary carbohydrates, including polysaccharides, oligosaccharides, and starches of plant origin. Only the microbiota harbouring our gut can ferment them and produce Short Chain Fatty Acids (SCFAs). SFCAs act as the primary energy source to support both the microbial growth and the gut cells. It also regulates optimal lipid and cholesterol metabolism besides colonic immunity.
But, when you continuously eat food low in complex carbohydrates, it alters gut pH and modifies the structure and metabolism of gut microbiota—reduced dietary carbohydrate results in the reduction of total SCFA. Also, an alteration in gut microbiome profile characterized by decreased Roseburia, the Eubacterium, and Bifidobacteria occurs.
Additionally, a protein-rich diet with a low proportion of carbohydrates also alters gut microbiome composition. The ratio of the abundance of Gram+ and Gram− bacteria gets ultimately reverses in the gut of both the obese and anorexic people.
Gut crisis when good microbes crash
Health remains the most valuable currency. If not realized on time, it can cost you a lot of your actual money. So, how the good microbes go up and down in an obese gut? Gut microbiome composition is extremely diverse between healthy individuals, lean, and overweight ones, characterized by the low bacterial richness in obese subjects.
High numbers of Firmicutes and low numbers of Bacteroidetes occur in obese people. The proportion of Bacteroidetes increases with low-calorie diet-based weight loss, thus, suggesting a tight association between the gut microbiota and body weight regulation. Less diversified gut flora during obesity becomes inefficient in consuming energy produced from metabolic processes. Altered gut flora in overweight people thus causes amplified production of energy from food. It also promotes the storage of fats by encouraging the formation of biological products required for the same.
Obesity-induced transformed intestinal flora also produces bacterial endotoxins, which pass into our circulation and cause inflammation and insulin resistance. Finally, leading to enhanced fat deposition and related complications. Alterations of the gut microbiome in initial life also boost the onset of obesity due to altered mechanisms regulating satiety/appetite.
Gram-negative bacteria, abundant in the gut of obese people, damage the gut epithelium and enhance the permeability of the intestinal wall. As a consequence, loads of bacterial endotoxins enter the blood circulation stimulating the production of molecules associated with obesity. Moreover, excessive gut barrier disruption can also result due to the activation of metabolic pathways that affect adipose tissue. This also aggravates the initial disorders and leads to a vicious cycle of detrimental processes.
Giving the microbes healthy nutrition
One can correct dysbiosis induced obesity by tracing the path back to healthy gut microbiota. Just correcting the proportions of healthy microbes can help you become lean. One can reform gut dysbiosis by several months of the regular low-energy diet, including intake of some micronutrients, prebiotics, and probiotics. Altered diet impacts the regulation of gene expression of the liver, muscle, and adipose tissue along with the alteration of gut microbiome composition. Regular intake of probiotics improves gut health by restoring the gut epithelium, healthy bloodstream, and controlling local inflammation19.
Antioxidants present in tea, like oolong tea polyphenols (OTP), mainly increase gut bacterial biodiversity with a higher number of Bacteroidetes and a low number of Firmicutes. They are thereby helping your gut experience the healthy flow of SCFAs once again. Intake of another prebiotic, galacto-oligosaccharide (GOS), encourages the abundance of Bacteroides, Ruminococcaceae, and Oscillibacter. It not only reduces the production of harmful bacterial metabolites but also brings down blood triglyceride levels.
Thus, probiotics and prebiotics like, GOS and OTP can be used to prevent obesity-related metabolic disorders through modification of the intestinal microbiota. Additionally, regular physical exercise also helps to lose weight. It also restores gut health by encouraging beneficial gut flora, which synthesizes SCFAs and controls the local inflammation. Another therapeutic option to treat obesity is through various surgical techniques, known as Bariatric surgery, which find a relation with alteration of gut flora and weight reduction and other health benefits.
Gut microbiome test: a helpful tool
The fact is that even modest weight loss can improve or prevent obesity-associated complications. For that, it is a prerequisite to have a ‘Gut microbiome test.’ It identifies your unique microbiome. State-of-the-art, ‘DNA sequencing technology,’ and algorithm-based data acquisition are used in this process. A prescription diet is formulated comprising of probiotics, and prebiotics based on the test results. Dietary changes increased physical activity, and lifestyle is the key to lose weight.